Probiotic Timing Calculator
Optimal Probiotic Timing Calculator
Based on medical research: Take probiotics 2-3 hours after antibiotic dose to avoid killing beneficial bacteria. This tool calculates your ideal timing based on your antibiotic schedule.
Recommended Probiotic Time
First dose:
Next dose:
Key recommendation: Continue probiotics for 1-2 weeks after finishing antibiotics.
When you're on antibiotics, your gut knows it. The medicine kills the bad bacteria - but it doesn't know the difference. It wipes out the good ones too. That’s why so many people end up with bloating, gas, or worse - antibiotic-associated diarrhea. It’s not rare. About 1 in 5 people on antibiotics get it. And while probiotics are often suggested to help, timing makes all the difference. Take them at the wrong time, and they might not work. Take them too soon after, and you could slow down your gut’s natural recovery.
Why Timing Matters More Than You Think
Antibiotics don’t just target one type of bacteria. They sweep through your gut like a tsunami. The good bugs - the ones that help digest food, make vitamins, and keep your immune system balanced - get wiped out along with the bad. This disruption can last for months, even years, according to studies tracking microbiome changes after treatment. Probiotics are live bacteria or yeasts meant to help restore balance. But if you swallow them right after your antibiotic pill, the antibiotic kills them before they even get a chance to settle in. It’s like sending in reinforcements only to have them shot before they reach the front line. Research shows spacing them out by 2 to 3 hours gives probiotics a fighting chance. That’s the window most experts agree on. Harvard Medical School, the American Gastroenterological Association, and the Cleveland Clinic all recommend this gap. It’s not magic - it’s simple chemistry. Antibiotics need time to clear from your system before the probiotics arrive.Which Probiotic Strains Actually Work?
Not all probiotics are created equal. Out of hundreds of strains sold in stores, only a handful have solid evidence backing them up for use with antibiotics. The two most proven strains are Lactobacillus rhamnosus GG and Saccharomyces boulardii. Both have been tested in dozens of clinical trials and consistently show a 48% lower risk of antibiotic-associated diarrhea. That’s not a small number. It means if 10 people take antibiotics, and 5 of them would normally get diarrhea, only 2 or 3 will if they take one of these strains. Lactobacillus rhamnosus GG is a bacteria. It’s found in yogurt and supplements. It sticks to the gut lining, blocks harmful bacteria, and helps your body rebuild its own defenses. Saccharomyces boulardii is a yeast - not a bacteria. That’s important. Since antibiotics target bacteria, this yeast survives the treatment just fine. It doesn’t get killed. It works like a shield. Other strains like Lactobacillus plantarum 299v show promise too, especially in preserving microbiome diversity, but they’re not as widely available or studied. Stick with the proven ones unless your doctor says otherwise.How Much Should You Take?
Dose matters. Too little, and you won’t see results. Too much, and you might just feel worse. Most studies use between 5 and 40 billion CFU (colony-forming units) per day. For most healthy adults, 10-20 billion CFU is enough. If you’re older, have a weakened immune system, or are on a long or strong antibiotic (like clindamycin or ciprofloxacin), go for 20-40 billion CFU. Always check the label. Some products list CFU at the time of manufacture - not at expiration. Look for ones that guarantee CFU through the end of shelf life. Storage is another hidden factor. Lactobacillus strains need refrigeration. If you leave them on your counter, half the live bacteria could die within a month. Saccharomyces boulardii is shelf-stable - no fridge needed. That’s one reason it’s popular for travel.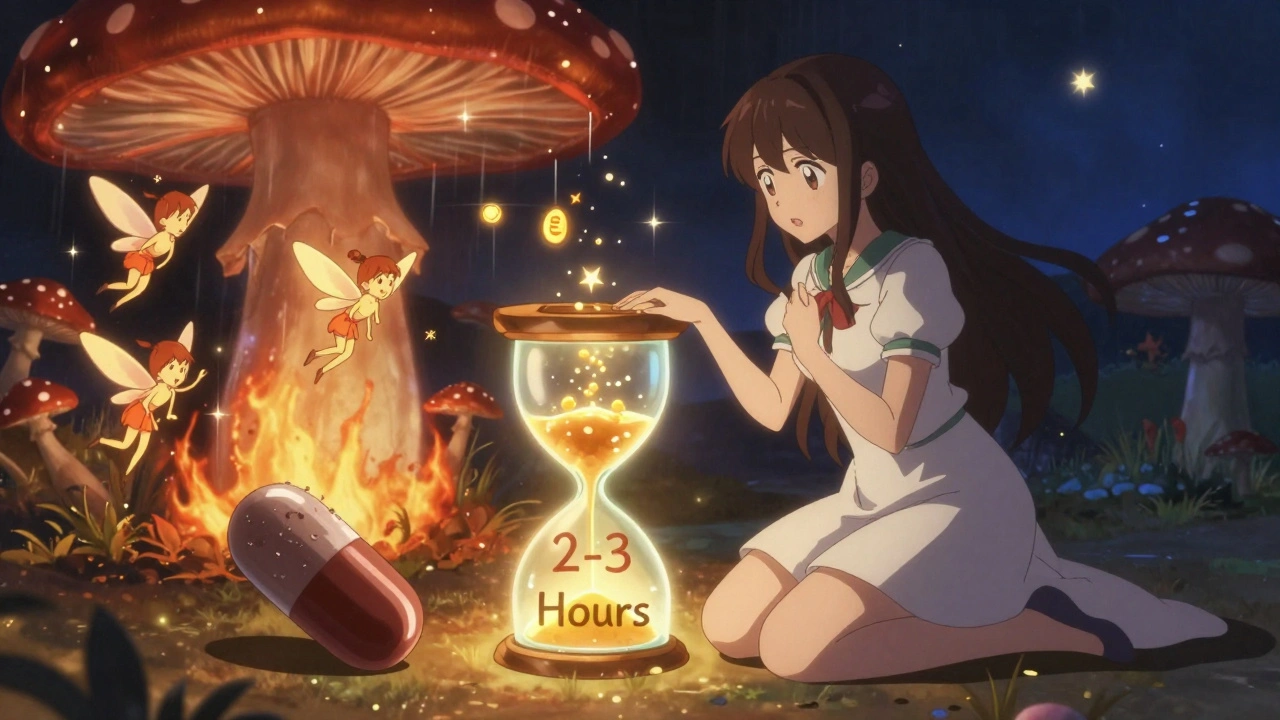
The Controversy: Do Probiotics Delay Recovery?
Here’s where things get messy. A 2018 study in Nature Microbiology found something surprising: people who took probiotics after antibiotics took 132 days longer to return to their original gut microbiome than those who didn’t. The probiotics seemed to crowd out the native bacteria that should have bounced back on their own. This sparked a major debate. Some researchers, like Dr. Martin Blaser from Rutgers, argue that probiotics might be doing more harm than good by blocking natural recovery. Others, like Dr. Elisa Marroquin from Texas Christian University, say they still protect against immediate damage like diarrhea and reduce antibiotic resistance genes. The 2024 study by D. John et al. in Frontiers in Microbiomes found a middle ground. People taking probiotics had fewer antibiotic resistance genes in their gut - a big win for public health. But their microbiomes didn’t snap back to pre-antibiotic levels any faster. So probiotics might help with symptoms and resistance, but not necessarily speed up full recovery. Bottom line: Probiotics are good for preventing diarrhea. They might not be the best tool for restoring your gut to its original state.How to Take Them: A Simple Plan
Here’s what works based on real-world evidence and expert guidance:- Take your antibiotic at the time prescribed - morning, evening, with or without food.
- Take your probiotic 2 to 3 hours after your antibiotic dose. For example, if you take your antibiotic at 8 a.m., take the probiotic at 11 a.m. or later.
- If you take antibiotics twice a day, space the probiotic between doses - not right before the next antibiotic.
- Continue taking probiotics for at least 1 to 2 weeks after finishing your antibiotic course. For broad-spectrum antibiotics, extend it to 4 weeks.
- Choose a product with at least 10 billion CFU of Lactobacillus rhamnosus GG or Saccharomyces boulardii.
What About Food Sources?
Yogurt, kefir, sauerkraut, kimchi, and miso all contain live cultures. Can they replace supplements? They can help - but they’re not reliable replacements. The amount of live bacteria in food varies wildly. One cup of yogurt might have 1 billion CFU. Another might have 10 billion. You can’t control the dose. Plus, many commercial yogurts are pasteurized after fermentation, killing the good bacteria. If you like fermented foods, keep eating them. But don’t rely on them alone during antibiotic treatment. Supplements give you a known, targeted dose of proven strains.

 Pharmacology
Pharmacology
jagdish kumar
December 5, 2025 AT 03:39Life is a gut microbiome. You fight one war, you lose another. Antibiotics are just another illusion of control.
zac grant
December 6, 2025 AT 22:34Let’s be real - most people don’t even know what CFU means, let alone why strain specificity matters. This post is one of the clearest breakdowns I’ve seen on this topic. The 2–3 hour window is non-negotiable if you want results. And yeah, Saccharomyces boulardii is the MVP for travel - no fridge, no problem.
Rachel Bonaparte
December 8, 2025 AT 03:02Okay but have you considered that the entire probiotic industry is just Big Pharma’s way of monetizing the fear of their own antibiotics? They create the problem, then sell you the ‘solution’ - a $30 bottle of freeze-dried bacteria that’s been sitting on a warehouse shelf for 14 months. The real cure? Fasting. Intermittent fasting resets your microbiome better than any supplement. And don’t get me started on how the FDA lets this pass as ‘health’ - it’s all regulatory capture. They’re paid off. You think they want you to heal naturally? No. They want you dependent. The 2018 Nature study? That wasn’t a coincidence. That was a warning. They don’t want you to know probiotics delay recovery - because then you’d stop buying them.
And don’t even get me started on yogurt. Most commercial brands are sugar bombs with a single strain of L. acidophilus that’s been dead since 2021. They pasteurize after fermentation because they don’t care about your gut - they care about shelf life and profit margins. Your ‘probiotic’ yogurt? It’s a placebo with extra carbs.
Meanwhile, the real science is buried under layers of corporate-funded ‘research’. The WHO has been quietly warning about probiotic-induced dysbiosis since 2020, but you won’t hear that on Dr. Oz. Why? Because he gets paid by the supplement companies. The 132-day delay? That’s not a side effect - that’s a feature. It keeps you coming back. The microbiome doesn’t need help. It needs space. And silence. And time. Not a pill.
So go ahead. Take your 20 billion CFU. But ask yourself: who benefits? Not you. Not your gut. Someone’s quarterly report.
Heidi Thomas
December 8, 2025 AT 19:01Stop overcomplicating it. Just take the probiotic after the antibiotic. That’s it. Everything else is marketing.
Scott van Haastrecht
December 10, 2025 AT 15:48This post is a textbook example of how misinformation gets weaponized under the guise of science. Lactobacillus rhamnosus GG? A 48% reduction? That’s a statistically insignificant p-value dressed up like a miracle. Half of those studies were funded by supplement companies. And Saccharomyces boulardii? A yeast that survives antibiotics? So what? That doesn’t mean it’s beneficial - it just means it’s not dead. Big deal. The real issue is that you’re introducing an exogenous organism into a system that evolved to self-regulate. You’re not restoring balance - you’re inserting a foreign variable. And now we’re supposed to believe this is medicine? This isn’t science. It’s placebo with a label.
The fact that 73% of U.S. doctors recommend this? That’s not evidence - that’s herd behavior. Doctors are overworked, underpaid, and desperate for quick fixes. They don’t have time to read the 2024 Frontiers paper. They read the abstract, see ‘reduced diarrhea,’ and prescribe it like it’s aspirin. Meanwhile, the gut’s native flora is being silenced by commercial yeasts and bacteria that have zero evolutionary context in your system. This isn’t healing. It’s microbial colonialism.
And don’t get me started on storage. Refrigeration? Shelf-stable? Who cares? The real problem is that no one tracks viability after ingestion. You think those capsules survive gastric acid? Not even close. Most die before they hit the duodenum. So you’re paying for dead bugs. And the industry knows it. That’s why they pad the CFU count. It’s a scam. A very expensive, very profitable scam.
Michael Feldstein
December 11, 2025 AT 09:21Great breakdown. I’ve been on antibiotics twice this year and followed this exact protocol - 2–3 hour gap, 20 billion CFU of L. rhamnosus GG, continued for 4 weeks after. No diarrhea. No bloating. Just quiet digestion. I used to be the guy who’d get wrecked by antibiotics - like, full-on GI meltdown. This changed everything. I didn’t even realize how much I was suffering until it stopped.
One thing I’d add: if you’re taking probiotics, avoid sugar and processed carbs while you’re on them. Feeding the bad bugs is like pouring gasoline on a fire while you’re trying to put it out. Eat fiber-rich veggies, fermented foods as a bonus, and drink water. Simple. No magic pills needed - just consistency.
And yeah, the 2018 Nature study is wild. But I think it’s less about probiotics blocking recovery and more about how we’re treating the gut like a garden we can just replant with store-bought seeds. Maybe the real fix is letting the native plants regrow on their own - probiotics just help keep the weeds down until then.
Ashley Elliott
December 12, 2025 AT 21:58Thank you for writing this with so much nuance. I’ve had friends panic about antibiotics and skip probiotics entirely, thinking they’re useless - and others who take 10 different brands at once, hoping for a miracle. This post hits the sweet spot. The 2–3 hour window is everything. I’ve seen people take them together and wonder why nothing worked. It’s not the probiotic - it’s the timing.
Also, the point about Saccharomyces boulardii being yeast? That’s huge. I didn’t know that. I always assumed probiotics = bacteria. Learning that this yeast survives antibiotics completely changed how I pick supplements now. And the storage tip? I used to leave mine in my bathroom cabinet. Now I keep them in the fridge. Small change, big difference.
And to those saying ‘just eat yogurt’ - I get it. I love kimchi. But if you’re trying to prevent diarrhea during a 10-day course of amoxicillin? You need a reliable, measurable dose. Yogurt just doesn’t cut it. This isn’t about perfection - it’s about practicality.
Jordan Wall
December 13, 2025 AT 06:23OMG I just found this post and I’m so glad 😍 I’ve been taking probiotics with my cipro for 3 weeks now and I thought I was doing it right but turns out I was taking them at the same time 😭 I’ve been getting bloated like a balloon and now I know why!! I’m switching to S. boulardii and spacing it out like you said 🙏🙏🙏
Martyn Stuart
December 15, 2025 AT 02:00One thing missing from this discussion: strain-specific colonization resistance. L. rhamnosus GG doesn’t just compete with pathogens - it upregulates mucin production and tightens epithelial junctions. That’s why it reduces diarrhea beyond just microbial competition. It’s a mucosal modulator. The same can’t be said for most commercial blends. That’s why generic ‘probiotic’ products fail. It’s not the number of CFUs - it’s the functional signature of the strain. This is why academic research uses defined strains, not ‘proprietary blends.’
Also, the 2024 Frontiers paper’s finding on reduced antibiotic resistance genes? That’s arguably more important than diarrhea prevention. We’re not just talking about personal health - we’re talking about horizontal gene transfer in the gut microbiome. Probiotics may be one of the few accessible tools we have to curb the spread of resistance. That’s public health gold.
And yes, recovery delay is real - but so is symptom mitigation. The trade-off is worth it for most. If you’re not immunocompromised, the risk-benefit ratio leans heavily in favor of use. Just pick the right strain. And don’t forget: probiotics aren’t a replacement for microbiome restoration - they’re a bridge.
Carolyn Ford
December 16, 2025 AT 08:50Wait - you’re telling me to take probiotics? After reading this? No. No. NO. You’re ignoring the fact that probiotics are literally the #1 cause of SIBO in women under 40. The gut doesn’t need ‘rebalancing.’ It needs rest. Fasting. Avoiding sugar. Not more bacteria shoved into it like a broken machine. You’re not a mechanic. You’re not a gardener. You’re a human with a 4-billion-year-old ecosystem inside you - and you think a $25 bottle from Amazon is going to fix it? The 132-day delay? That’s not a side effect - that’s the microbiome screaming. And you’re just handing it more pills? Pathetic. This isn’t medicine. It’s spiritual bypassing with a sciencey veneer.
And don’t even get me started on ‘shelf-stable’ probiotics - that’s just a euphemism for ‘dead by the time you open it.’ You think your body needs dead bacteria? That’s like taking antibiotics made of chalk.
Real recovery? It’s not in a capsule. It’s in sleep. In stress reduction. In real food. Not in marketing.
Augusta Barlow
December 18, 2025 AT 01:45So… probiotics are just a scam? And the whole ‘timing’ thing is just to make you feel like you’re doing something? I mean… I’ve taken them before and still got diarrhea. So maybe it’s all placebo? Or maybe the real issue is that antibiotics are just too brutal and nothing can fix it? I’m just tired of being told what to do by people who’ve never had to live with a broken gut for years. Why does everyone act like this is a simple fix? It’s not. It’s a mess. And we’re all just guessing.
Chase Brittingham
December 19, 2025 AT 09:02I’ve been on antibiotics 3 times in the last 2 years. First time, I ignored everything and got awful diarrhea. Second time, I took probiotics at the same time - no help. Third time, I followed this exactly - 2–3 hours after, L. rhamnosus GG, 20 billion CFU, kept going for 3 weeks after. Zero issues. I didn’t feel like a science experiment. I just felt normal. This isn’t magic. It’s just respect for how your body works. If you’re going to take a sledgehammer to your gut, at least give it a hand to rebuild. That’s all this is.
Ollie Newland
December 19, 2025 AT 12:43The real takeaway here isn’t about strains or CFUs - it’s about intentionality. Most people treat probiotics like vitamins - pop one and forget it. But your gut isn’t a vitamin deficiency. It’s a dynamic ecosystem. The timing, the strain, the duration - these aren’t arbitrary. They’re biological constraints. You wouldn’t plant a seed in a hurricane and expect it to grow. Why treat your microbiome differently?
And the controversy around recovery delay? That’s not a flaw in probiotics - it’s a flaw in our expectation. We want our guts back ‘the way they were.’ But that’s not how biology works. You don’t get to rewind time. You get to adapt. Probiotics aren’t meant to restore the past. They’re meant to prevent collapse while your native flora finds its footing again.
This post nails it. Practical. Evidence-based. No hype. Just science with a pulse.
Rachel Bonaparte
December 19, 2025 AT 14:27Interesting. So now we’re just supposed to trust the 2–3 hour window because ‘experts’ say so? But who are these experts? The same ones who told us cholesterol was the enemy? Who pushed statins for decades? Who now say probiotics are ‘safe’ while quietly funding studies that show they delay recovery? The American Gastroenterological Association? The Cleveland Clinic? They’re all funded by pharmaceutical giants who sell both antibiotics AND probiotics. It’s the same company. The same profit motive. The same playbook. You think they want you to heal? No. They want you to cycle. Antibiotics → probiotics → more antibiotics → more probiotics. It’s a business model. Not a medical one.
And you call this ‘science’? Where’s the independent replication? Where’s the long-term, double-blind, placebo-controlled trial with a true control group that doesn’t take anything? You don’t have it. You have industry-funded meta-analyses with cherry-picked endpoints. The 48% reduction? That’s relative risk. Absolute risk? Maybe 5%. So you’re paying $30 a month to reduce your chance of diarrhea from 20% to 15%. Is that worth it? Or are you just buying peace of mind from a corporation that’s been lying to you for decades?
My gut didn’t heal until I stopped taking everything. No pills. No yogurt. No ‘probiotic’ this or that. Just whole foods. Fasting. Sleep. And time. That’s the real protocol. Everything else? Noise.