It’s easy to think that taking a few extra pills - maybe an over-the-counter painkiller, a herbal supplement, or a new prescription - won’t cause trouble. But drug interactions don’t always announce themselves with a warning label. Sometimes, they creep in quietly, making you feel off, tired, dizzy, or just “not yourself.” And if you ignore those signs, what starts as mild discomfort can turn into a medical emergency overnight.
What Exactly Is a Drug Interaction?
A drug interaction happens when one substance changes how another substance works in your body. This could be another medication, a food like grapefruit, an herbal supplement like St. John’s wort, or even alcohol. The result? The drug might become less effective, too strong, or cause side effects you’ve never had before. About 60% of serious interactions involve two or more medications, according to pharmacology textbooks. Another 20% come from food or supplements, and the rest are tied to underlying health conditions like kidney or liver disease.The real danger isn’t just feeling weird - it’s that these interactions can lead to life-threatening reactions. In the U.S. alone, drug-related problems send 1.3 million people to the emergency room every year. Nearly 350,000 of those cases require hospitalization. And here’s the kicker: 40% of these reactions could have been prevented with better awareness.
Red Flags That Demand Immediate Emergency Care
If you’re taking multiple medications - especially for heart conditions, mental health, or chronic pain - you need to know the signs that mean call 911 right now.- Difficulty breathing or oxygen levels below 90%: If you’re gasping, wheezing, or your lips turn blue, this could be anaphylaxis. Pulse oximetry readings below 90% are a clear red flag.
- Swelling of the face, tongue, or throat: This isn’t just a rash. Angioedema can block your airway in as little as 15 minutes. If you feel like your throat is closing, don’t wait.
- Heart racing and blood pressure crashing: A heart rate over 120 beats per minute with systolic pressure below 90 mmHg signals shock. This is common in severe allergic reactions or serotonin syndrome.
- Seizures or loss of consciousness: If you or someone else has a seizure lasting more than two minutes, or can’t stay awake and responds poorly to questions (Glasgow Coma Scale under 13), get help immediately.
- High fever, stiff muscles, and extreme agitation: These are signs of serotonin syndrome or neuroleptic malignant syndrome - both rare but deadly. Temperatures above 41°C (106°F), muscle rigidity so severe you can’t move, and uncontrollable shaking mean you’re in critical condition.
These symptoms don’t wait. If you’re on antidepressants like SSRIs, pain meds like tramadol, or antipsychotics, and you’ve recently added something new - even a cold medicine or CBD oil - these reactions can happen fast. One Reddit user reported developing serotonin syndrome after a dentist gave them fentanyl while they were on an SSRI. They ended up in the ICU.
Symptoms That Need a Doctor Within 24 Hours
Not every interaction causes a crisis. But some warning signs mean you can’t just “wait and see.” These need a call to your doctor or a visit to urgent care within a day.- Widespread rash covering more than 30% of your body: Especially if it’s red, raised, and itchy. This could be DRESS syndrome - a severe drug reaction that can damage your liver, kidneys, or blood cells.
- Unexplained fever over 38.5°C (101.3°F) for more than two days: If you’ve started a new antibiotic, anticonvulsant, or blood pressure drug, this could be serum sickness or a delayed immune reaction.
- Unusual bruising, bleeding, or extreme fatigue: A sudden drop in platelets or hemoglobin could mean your bone marrow is being suppressed. This happens with some antibiotics, antivirals, or even NSAIDs.
- Yellow skin, dark urine, or right-side abdominal pain: These are signs of liver damage. ALT levels above 120 U/L are a red flag. Drug-induced liver injury is rare but can be silent until it’s advanced.
- Little or no urine output for 6+ hours with rising creatinine: Your kidneys might be shutting down. About 1 in 5 cases of sudden kidney failure in hospitals are caused by medications.
Many people brush these off. One survey found that 58% of patients waited more than 12 hours before calling their doctor - even after experiencing dizziness, nausea, or confusion. By then, the damage was often already done.
Who’s at Highest Risk?
You don’t have to be elderly to be at risk. But if you’re taking five or more medications, your chance of a dangerous interaction jumps to 57%. That’s not a small number - it’s the norm for many people with chronic conditions.Older adults are especially vulnerable. Nearly half of people over 65 take five or more drugs. But even younger people are at risk if they’re on:
- Warfarin (blood thinner)
- Digoxin (heart medication)
- Phenytoin (seizure drug)
- SSRIs or SNRIs (antidepressants)
- Statins (cholesterol drugs)
These drugs have what’s called a “narrow therapeutic index.” That means the difference between the right dose and a toxic one is tiny. A 20% change in blood levels can cause serious harm. One study found that interactions with these drugs caused 30% of all preventable hospitalizations.
What You Can Do Right Now
You don’t need to be a pharmacist to protect yourself. Here’s what works:- Keep a current list of everything you take: Include prescriptions, OTC meds, vitamins, herbs, and even recreational substances like alcohol or cannabis. Write down the dose and how often you take it.
- Use a drug interaction checker: Tools like Drugs.com or Lexicomp let you enter all your meds and get instant alerts. Don’t skip supplements - 18% of serious interactions involve them.
- Ask your pharmacist every time you pick up a new prescription: They’re trained to spot conflicts. Many don’t even charge for this.
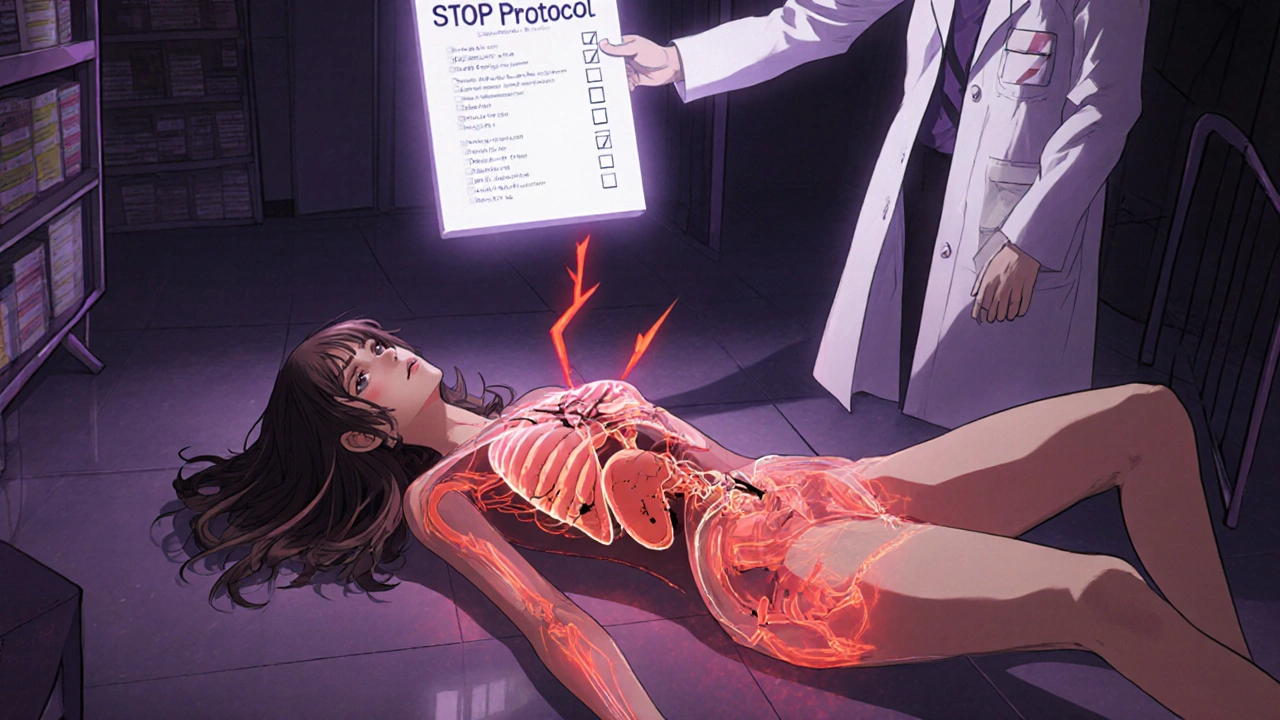
- Use the STOP protocol: If you suspect an interaction, Stop taking the medication, Telephone your provider, Observe your symptoms, and Present all your medication containers at your appointment.
One study showed that patients who called poison control within an hour of noticing symptoms avoided ER visits 89% of the time. That’s huge.
Why Most People Miss the Signs
A 2022 study found that 68% of patients couldn’t recognize serious interaction symptoms from the tiny print on their medication leaflets. That’s not their fault. The language is confusing, the symptoms are vague, and the warnings are buried.Doctors are overwhelmed too. In one survey, nearly half of primary care physicians said they ignore interaction alerts because they get too many - a problem called “alert fatigue.” So you can’t rely on your doctor to catch everything. You have to be your own advocate.
Real people share stories online: someone took melatonin with an SSRI and had violent nightmares. Someone else took ibuprofen with a blood pressure pill and ended up in the hospital with kidney failure. These aren’t rare. They’re preventable.
What Happens After You Seek Help?
When you go to the ER or call your doctor, they’ll likely:- Ask for your complete medication list
- Run blood tests (liver, kidney, electrolytes, drug levels)
- Stop the suspected drug(s) - this is called a “dechallenge”
- Monitor your symptoms for improvement
- Reintroduce the drug later, if needed, to confirm the cause - this is a “rechallenge,” used only in controlled settings
Doctors use a tool called the CIOMS scale to decide if a reaction is definitely caused by a drug. It looks at timing, whether symptoms disappeared after stopping the drug, and whether they came back when it was restarted. This isn’t guesswork - it’s science.
Final Thought: Don’t Wait Until It’s Too Late
Medications save lives. But they can also hurt you - especially when you don’t know what you’re mixing. The most dangerous interactions aren’t the ones you read about in textbooks. They’re the ones you ignore because you think you’re “just tired” or “a little dizzy.”If you’re on multiple drugs - especially if you’re over 65, have kidney or liver issues, or take heart, mental health, or seizure medications - treat any new or unusual symptom as a warning. Don’t wait. Don’t hope it goes away. Call your doctor. Go to urgent care. Or if it’s serious, call 911.
It’s not paranoia. It’s protection.
What are the most common drugs that cause dangerous interactions?
The most dangerous interactions often involve drugs with a narrow therapeutic index - meaning small changes in blood levels can cause big problems. These include warfarin (blood thinner), digoxin (heart medication), phenytoin (seizure control), lithium (mood stabilizer), and certain antibiotics like vancomycin. SSRIs and SNRIs (antidepressants) also commonly interact with pain relievers, migraine meds, and herbal supplements like St. John’s wort, leading to serotonin syndrome.
Can over-the-counter medications cause serious interactions?
Absolutely. Common OTC drugs like ibuprofen, naproxen, and acetaminophen can interact with blood pressure meds, blood thinners, and kidney medications. Even cold and allergy medicines containing pseudoephedrine or dextromethorphan can cause dangerous spikes in blood pressure or serotonin syndrome when mixed with antidepressants. Many people assume OTC means safe, but that’s not true when combined with other drugs.
Is it safe to take herbal supplements with prescription drugs?
Not without checking. Herbal supplements like St. John’s wort, garlic, ginkgo, and ginger can interfere with how your body processes medications. St. John’s wort, for example, can reduce the effectiveness of birth control, antidepressants, and HIV drugs. Garlic and ginkgo can increase bleeding risk when taken with warfarin. About 18% of serious drug interactions involve herbal products, according to the National Institutes of Health.
What should I do if I think I’m having a drug interaction?
Use the STOP protocol: Stop taking the suspected medication immediately. Telephone your doctor or poison control (1-800-222-1222 in the U.S. and Canada). Observe your symptoms closely - write down what you feel, when it started, and how it’s changing. Then, Present all your medication containers - including bottles, supplements, and OTC drugs - to your healthcare provider. This helps them identify the culprit quickly.
Can drug interactions happen even if I’ve been taking the same meds for years?
Yes. Your body changes over time. As you age, your liver and kidneys process drugs differently. New health conditions, like kidney disease or thyroid problems, can also change how drugs behave. Even adding a new vitamin or changing your diet (like eating more grapefruit) can trigger an interaction you never had before. Just because something was safe last year doesn’t mean it’s safe today.
How can I prevent drug interactions in the future?
Keep a written or digital list of every medication and supplement you take - including doses and times. Review it with your pharmacist every time you get a new prescription. Use a free drug interaction checker like Drugs.com or Lexicomp. Never start a new supplement without asking your doctor or pharmacist. And always tell every healthcare provider you see - including dentists and specialists - about everything you’re taking.

 Pharmacology
Pharmacology
Olivia Currie
November 29, 2025 AT 22:33This post literally saved my life. I was taking melatonin with my SSRI and had these terrifying nightmares - thought I was going crazy. Then I read this and realized it was the combo. Stopped it immediately and called my doctor. Thank you for putting this out there. 🙏
Curtis Ryan
November 30, 2025 AT 17:19OMG YES I’M SO GLAD THIS EXISTS!! I just started statins and took ibuprofen for a headache and felt like I was gonna pass out. Went to urgent care and they said it was probably the combo. I didn’t even know OTC stuff could do that. My bad for assuming ‘over the counter’ = ‘safe as water’ 😅
Rajiv Vyas
December 2, 2025 AT 08:48They’re scaremongering again. You know who really controls drug safety? Big Pharma. They make the warnings so confusing so you’ll keep buying new pills instead of just using turmeric and sunlight like nature intended. This whole thing is a money grab. I haven’t taken a prescription in 7 years and I’m 92 and still hiking. You’re being manipulated.
farhiya jama
December 3, 2025 AT 05:26Ugh. I read this whole thing and now I’m paranoid I’m gonna die from my multivitamin. I already take 12 things. I’m just gonna… stop everything. And nap. Forever.
Astro Service
December 3, 2025 AT 21:05Why are we even talking about this? In America we don’t need this stuff. If you’re dumb enough to mix drugs, you deserve what you get. We got guns and freedom, not pill police. Stop whining and take responsibility.
DENIS GOLD
December 4, 2025 AT 22:04Wow. So the solution to every medical problem is ‘call a doctor’? What a revolutionary idea. Next they’ll tell us to brush our teeth. 🤡
Ifeoma Ezeokoli
December 6, 2025 AT 01:38Thank you for writing this with so much heart. I’m a nurse in Lagos and I see this every day - people mixing traditional herbs with antiretrovirals, thinking ‘it’s natural so it’s fine.’ This is exactly the kind of clarity we need. Please share this with more communities. 💛
Daniel Rod
December 6, 2025 AT 22:20It’s wild how we’re taught to trust medicine blindly, but never taught how to read the fine print. We’re supposed to be experts on our own bodies, yet no one gives us the tools. Maybe the real problem isn’t the drugs - it’s the system that leaves us alone in the dark. 🌱
gina rodriguez
December 8, 2025 AT 06:02I keep a printed list of everything I take in my wallet. I show it to every doctor, even the dentist. It’s saved me twice already. Small habit, huge impact. You’ve got this 💪
Sue Barnes
December 9, 2025 AT 11:43If you’re taking more than 3 meds, you’re probably just lazy. Stop being a medical tourist. Get your life together. This post is just enabling people who don’t want to be healthy.
jobin joshua
December 10, 2025 AT 08:43Bro I took 2 Advil with my blood pressure med and my hands turned purple 😳 I thought I was dying. Called poison control and they said ‘you’re lucky you’re alive.’ Now I use the Drugs.com checker every time. Don’t be like me.
Sachin Agnihotri
December 12, 2025 AT 02:46My mom had liver damage from a statin and garlic supplement - she didn’t even know garlic could do that. Now she uses the STOP protocol religiously. I printed it out and taped it to her fridge. 🙏
Diana Askew
December 13, 2025 AT 15:04They didn't mention the real villain: the FDA. They're paid off. That’s why you never hear about the 100,000 people who die every year from 'approved' drugs. This post? Just a distraction. Wake up. 🚨