When you’re on warfarin, even a simple pain reliever can turn dangerous. That’s not a scare tactic-it’s science. Warfarin, a blood thinner prescribed for conditions like atrial fibrillation or deep vein thrombosis, keeps your blood from clotting too easily. But when you add an NSAID-like ibuprofen, naproxen, or even aspirin-to that mix, you’re not just doubling up on pain relief. You’re stacking two mechanisms that can cause serious, sometimes deadly, bleeding.
How Warfarin Works
Warfarin doesn’t thin your blood like water. It blocks vitamin K, a key ingredient your liver needs to make clotting factors-specifically factors II, VII, IX, and X. Without enough active clotting factors, your blood takes longer to form clots. That’s why doctors monitor your INR (International Normalized Ratio), a test that measures how long it takes your blood to clot. A normal INR is around 1.0. For someone on warfarin, the target is usually between 2.0 and 3.0. Go above 4.0, and your bleeding risk spikes.
What makes warfarin tricky is how sensitive it is. Small changes in diet, other medications, or even your liver function can throw your INR off. That’s why regular blood tests are non-negotiable. But when you add an NSAID, you’re not just nudging the scale-you’re tipping it.
How NSAIDs Interfere
NSAIDs-nonsteroidal anti-inflammatory drugs-are everywhere. You take them for headaches, arthritis, menstrual cramps, or back pain. They work by blocking enzymes called COX-1 and COX-2. COX-2 is linked to inflammation and pain. COX-1? That’s the one that protects your stomach lining and helps platelets stick together to stop bleeding.
When NSAIDs block COX-1, they reduce thromboxane A2, a chemical that tells platelets to clump together. No thromboxane? Platelets can’t do their job. Your blood takes longer to clot, even without warfarin. Combine that with warfarin’s effect on clotting factors, and you’ve got a one-two punch.
And it’s not just platelets. NSAIDs also damage the stomach lining by reducing protective prostaglandins. That’s why people on long-term NSAIDs get ulcers. When warfarin is in the picture, those ulcers don’t just hurt-they bleed. And they bleed hard.
The Numbers Don’t Lie
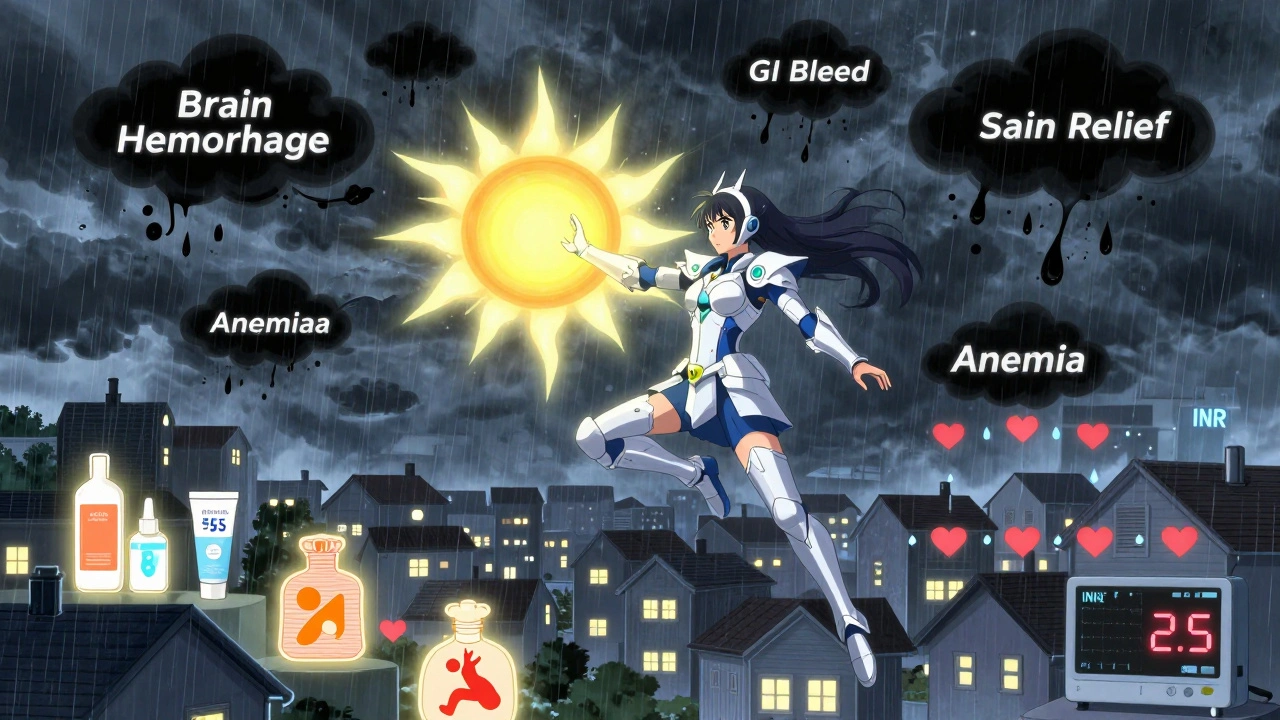
Studies have quantified exactly how dangerous this combo is. One large study found that people taking warfarin and an NSAID were more than twice as likely to bleed compared to those on warfarin alone. That’s a 2.09 times higher risk.
But not all NSAIDs are equal. Naproxen? It raised bleeding risk by 4.1 times. Diclofenac? 3.3 times. Ibuprofen? Still dangerous-at 1.79 times higher. Meloxicam? Even though it’s often considered “gentler,” it was linked to significant INR spikes in patients already on warfarin.
The bleeding isn’t just in your stomach. Brain bleeds (intracranial hemorrhage) became 3.22 times more likely. Lung bleeds? Up 36%. Urinary tract bleeds? 57% higher. And nearly one in three people on this combo developed anemia from hidden, slow bleeding.
One study tracked 98 warfarin users who started an NSAID. Almost 40% of them saw their INR jump by 15% or more-enough to push them into dangerous territory. That’s not a fluke. That’s a pattern.

Who’s at Highest Risk?
It’s not just about taking both drugs. Certain factors make the risk worse:
- High warfarin dose-Over 40 mg per week. That means you’re already on the edge of your therapeutic range.
- Low baseline INR-If your INR was low before starting the NSAID, your body had less room to handle the extra anticoagulant effect.
- Other medications-Antibiotics, antifungals, or even some herbal supplements can interact with warfarin, making NSAIDs even more dangerous.
- Age and history of GI issues-Older adults and those with past ulcers or GI bleeding are at the highest risk.
One study showed that patients taking warfarin and meloxicam had a statistically significant spike in INR-even when the dose was low. That’s a red flag. Meloxicam isn’t safer. It’s just different.
What About Newer Blood Thinners?
You might think switching to a DOAC-like apixaban or rivaroxaban-makes this problem go away. It doesn’t. While some studies show slightly lower bleeding risk with DOACs compared to warfarin when NSAIDs are added, the danger is still there.
A 2018 study on dabigatran found that NSAID users had significantly higher rates of major bleeding, even if the increase wasn’t statistically different from warfarin users. And here’s the kicker: 60% of those bleeds weren’t in the gut-they were in the brain, lungs, or elsewhere. That means NSAIDs can cause bleeding anywhere in your body, not just your stomach.
The bottom line? No blood thinner is safe with NSAIDs. Not warfarin. Not apixaban. Not rivaroxaban. Not dabigatran.
What Should You Do Instead?
If you’re on warfarin and need pain relief, here’s what actually works:
- Acetaminophen (Tylenol)-Up to 3,000 mg per day is generally safe. It doesn’t affect platelets or the stomach lining. It’s your best bet for mild to moderate pain.
- Topical pain relievers-Gels, creams, or patches with diclofenac or menthol. They deliver relief locally with almost no systemic absorption. That means they don’t touch your blood.
- Physical therapy-For joint or muscle pain, movement and strengthening can reduce pain long-term without drugs.
- Cold or heat therapy-Simple, effective, and zero interaction risk.
If your doctor insists on an NSAID-for severe arthritis, for example-then you need a plan:
- Use the lowest dose for the shortest time possible.
- Take it with food to reduce stomach irritation.
- Get a proton pump inhibitor (PPI) like pantoprazole 40 mg daily to protect your stomach lining.
- Check your INR within 3 to 5 days after starting the NSAID, then weekly until stable.
- Watch for signs of bleeding: black or tarry stools, bright red blood in stool, unusual bruising, headaches, dizziness, or blood in urine.
Why Do Doctors Still Prescribe This Combo?
It’s not because they don’t know the risks. They do. But pain is urgent. Patients demand relief. And sometimes, the alternative isn’t available or effective.
Still, studies show that nearly 3 out of 10 warfarin users get an NSAID prescription within a year. That’s a massive gap in care. Many of these prescriptions are unnecessary. Many are given without INR checks. Many are given without gastroprotection.
It’s preventable. It’s avoidable. And too many people end up in the ER because of it.
Bottom Line
Warfarin and NSAIDs don’t just interact-they amplify each other’s dangers. The risk isn’t small. It’s big. And it’s well-documented. You don’t need to guess. You don’t need to hope. You need to act.
If you’re on warfarin, skip the ibuprofen. Skip the naproxen. Skip the aspirin unless your cardiologist specifically told you to take it for heart protection. Reach for acetaminophen. Talk to your pharmacist. Ask about topical options. Push for physical therapy.
And if you’re told to take an NSAID anyway? Demand a plan. Ask for a PPI. Ask for an INR check in 3 days. Ask for a follow-up. Your life depends on it.
This isn’t just a drug interaction. It’s a warning sign. And if you ignore it, you’re gambling with your health.

 Pharmacology
Pharmacology
Cyndy Gregoria
December 4, 2025 AT 12:46Just got back from my PT session and I swear, movement is the real painkiller. No pills, no risks. If you're on warfarin, this is your new best friend.
Adrianna Alfano
December 6, 2025 AT 07:08I didn't know NSAIDs could mess with INR so badly. My grandma's on warfarin and she's been popping ibuprofen for years... I'm calling her right now. Thanks for this.
May .
December 7, 2025 AT 06:57Acetaminophen is fine
Akash Sharma
December 7, 2025 AT 21:26This is one of those posts that makes you realize how little we actually know about the meds we take daily. I've been on warfarin for 7 years now, and I thought NSAIDs were just a "maybe" thing. Turns out, it's not even a gray area-it's a red flag with flashing sirens. The part about meloxicam was eye-opening. I always assumed "gentler" meant safer, but no, it's just a different kind of danger. And the fact that 40% of people on this combo saw their INR jump by 15% or more? That's not statistical noise-that's a ticking clock. I used to take naproxen for my knee, thinking it was just a minor thing. Now I use ice packs and a TENS unit. I also started tracking my INR like a hawk after I read this. I didn't even know bleeding could happen in your lungs or brain from something as "harmless" as a pain reliever. And honestly, the biggest shocker? That 3 out of 10 warfarin users still get NSAIDs prescribed. That's not negligence, that's systemic. Doctors are overworked, patients are in pain, and somewhere in the middle, the science gets lost. I wish every pharmacy had a mandatory sticker on NSAID bottles: "DANGER: MAY BLEED YOU OUT IF YOU'RE ON WARFARIN." And why isn't there a blood thinner app that flags NSAIDs in your medication list? It's 2025. We have AI that writes poetry but can't warn you not to kill yourself with ibuprofen. I'm not mad, I'm just disappointed. And now I'm telling everyone I know who's on anticoagulants. This isn't just medical advice-it's survival info.
Palanivelu Sivanathan
December 8, 2025 AT 08:43So... we're all just one ibuprofen away from a hemorrhagic nightmare?? 😱 I mean, I get it, but also... is anyone else just tired of being told every little thing will kill you? I'm on warfarin, I want to feel better, not live in a bubble. 🤷♂️
Joanne Rencher
December 9, 2025 AT 09:33Wow. So many people die because they don't read the fine print. It's not rocket science. You're basically asking for trouble.
Siddharth Notani
December 10, 2025 AT 07:31As a clinical pharmacist in Mumbai, I've seen this exact scenario unfold too often. Patients come in with meloxicam prescriptions and no INR check in months. The cultural belief that "natural pain relief" means safe is dangerous. We've started handing out laminated cards with acetaminophen alternatives and topicals-simple, low-cost, life-saving. Also, remind your doctor: if they prescribe NSAIDs, they must document the risk discussion. It's not optional. It's standard of care.
Storz Vonderheide
December 10, 2025 AT 08:57Just want to add-topical diclofenac gel is a game-changer. I’ve been using it for shoulder pain while on rivaroxaban. Zero INR spikes, zero stomach issues. The key is local delivery. Systemic absorption is the killer. Also, if you’re on a DOAC and think you’re safe with NSAIDs, you’re not. The data is clear: bleeding risk still rises. Just less than warfarin. But not zero. So please, don’t assume.
Casey Lyn Keller
December 10, 2025 AT 13:19Anyone else think this is all part of a Big Pharma scheme to push more expensive meds? Warfarin’s cheap. DOACs? Not so much. And now they’re telling us NSAIDs are dangerous? Convenient.
Jessica Ainscough
December 11, 2025 AT 20:43My mom was on warfarin after her valve replacement. She started taking Aleve for her arthritis and ended up in the ER with a GI bleed. She’s fine now, but it scared the hell out of us. This post saved me from making the same mistake with my dad. Thank you.
Cristy Magdalena
December 13, 2025 AT 19:15I just cried reading this. My brother died from a brain bleed after taking Advil for a headache. He was on warfarin. No one warned him. No one told him. And now I have to live with that. Please, if you're on blood thinners-listen. This isn't fearmongering. It's a funeral waiting to happen.
dan koz
December 14, 2025 AT 14:58Man, this is why I don't trust American doctors. Here in Lagos, we just use ginger tea and heat packs. No pills, no problems. Why are you all so dependent on chemicals?
Mark Gallagher
December 14, 2025 AT 16:33You people are ridiculous. This is why America is falling apart. You can't even take a painkiller without a 2000-word essay. Acetaminophen? That's liver poison. NSAIDs? Fine if you're not a hypochondriac. Get a grip. Your INR is not a magic number. It's a guideline. And if you're too scared to take ibuprofen, maybe you shouldn't be on warfarin in the first place. Stop coddling yourselves.