Besifloxacin PK/PD Calculator
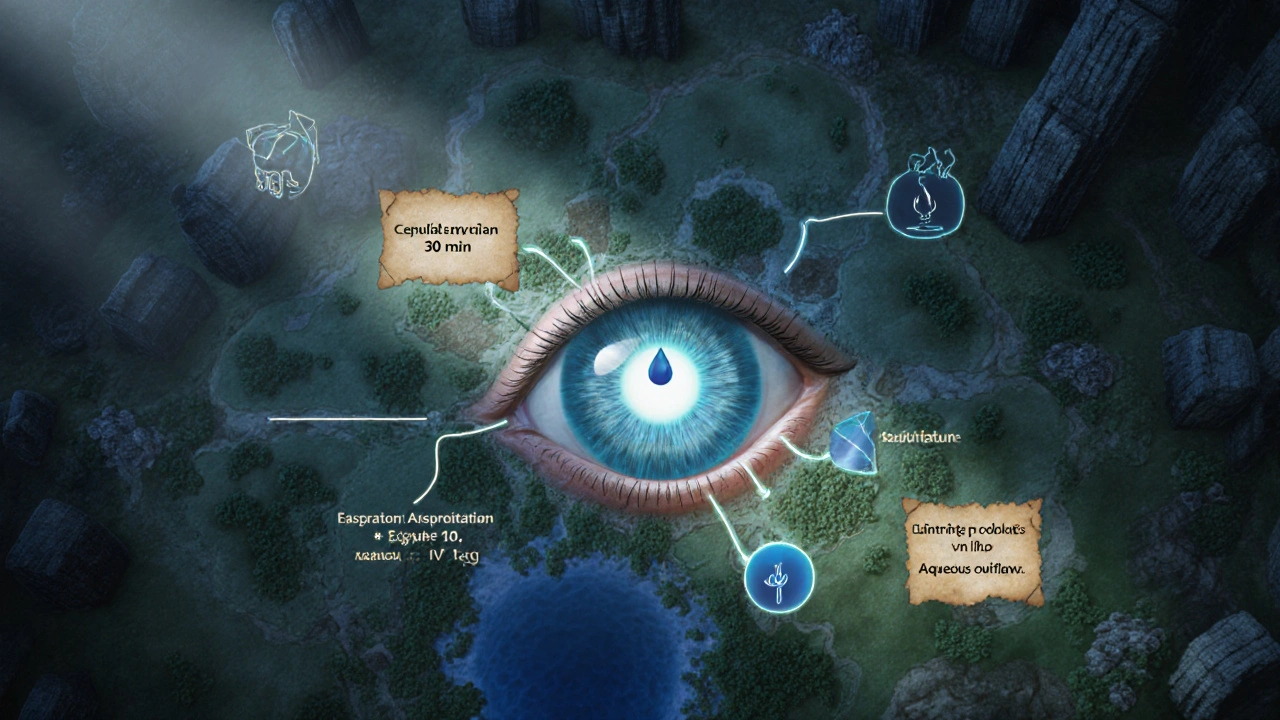
The calculator determines if besifloxacin's peak concentration (Cmax) is sufficient relative to the pathogen's MIC (Minimum Inhibitory Concentration). For fluoroquinolones, a Cmax/MIC ratio ≥ 8 is typically required for optimal bactericidal activity. Based on clinical data, besifloxacin achieves Cmax = 1.5 µg/mL in aqueous humor within 30 minutes of application.
Enter the MIC value for the bacterial strain (in µg/mL)
Besifloxacin is a fourth‑generation fluoroquinolone formulated exclusively for ophthalmic use. Developed to tackle bacterial conjunctivitis and keratitis, it delivers potent activity against Gram‑positive and Gram‑negative pathogens while minimizing resistance development.
Why a Technical Overview Matters
Clinicians and pharmacists often receive the drug’s brand name, but they need to understand how the molecule behaves inside the eye and how that translates into bacterial kill. This guide breaks down absorption, distribution, metabolism, and elimination (ADME) and then links those numbers to the drug’s pharmacodynamic (PD) profile, so you can predict therapeutic success and spot potential pitfalls.
Chemical Profile and Class Context
The molecule belongs to the Fluoroquinolone class, characterized by a fluorine atom at C‑6 and a cyclopropyl group that enhances DNA gyrase inhibition. Besifloxacin’s molecular weight is 387.4g/mol, pKa≈5.8 (basic), and it is lipophilic enough (logP≈2.1) to cross corneal epithelium but still water‑soluble for a clear ophthalmic suspension.
Pharmacokinetics (PK)
Because the drug is applied topically, systemic exposure is negligible. The PK parameters of interest are ocular concentrations over time.
Absorption - From Drop to Aqueous Humor
After a single 0.5% (5mg/mL) drop, peak concentrations (Cmax) in the aqueous humor reach about 1.5µg/mL within 30minutes (Tmax). The besifloxacin pharmacokinetics are driven by rapid corneal penetration and limited precorneal drainage, thanks to the viscous vehicle and a preservative‑free formulation.
Distribution - Where Does It Go?
Distribution is chiefly limited to the anterior segment. Measured concentrations in conjunctival tissue exceed 2µg/mL, while the corneal stroma retains 0.8‑1.2µg/mL for up to 6hours. Protein binding in tear fluid is low (<10%), allowing free drug to interact with bacterial targets.
Metabolism - Is It Broken Down?
Besifloxacin undergoes virtually no metabolic transformation in ocular tissues. Enzyme assays show <0.5% conversion to minor metabolites, meaning the parent drug is responsible for all activity.
Elimination - How Long Does It Stay?
Elimination from the eye occurs primarily via aqueous outflow. The elimination half‑life (t½) in the aqueous humor is reported at 3.0‑3.5hours, supporting a twice‑daily dosing regimen for most infections. Minimal systemic clearance (<0.1% of dose) eliminates concerns about drug‑drug interactions.
Pharmacodynamics (PD)
PD describes the drug’s effect on bacteria. For besifloxacin, the key metrics are minimum inhibitory concentrations (MIC) and the ratio of drug exposure to MIC.
Mechanism of Action
Besifloxacin, like other fluoroquinolones, binds to bacterial DNA gyrase (topoisomeraseII) and topoisomeraseIV, halting DNA replication and transcription. Its dual‑target affinity reduces the likelihood of resistance, especially against Staphylococcus aureus and Pseudomonas aeruginosa.
MIC Values - How Potent Is It?
Typical MIC ranges (µg/mL) for common ocular pathogens are:
- Staphylococcus aureus: 0.06-0.12
- Streptococcus pneumoniae: 0.03-0.06
- Haemophilus influenzae: 0.03-0.12
- Pseudomonas aeruginosa: 0.25-0.5
These values sit well below the achieved aqueous concentrations, giving a healthy margin of safety.
PK/PD Index - The Critical Ratio
For fluoroquinolones, the “AUC/MIC” (area under the concentration‑time curve divided by MIC) predicts efficacy. Studies show that an AUC/MIC>30 is needed for bactericidal activity. With a typical dosing schedule (0.5% drop twice daily), the calculated AUC in the aqueous humor is ~12µg·h/mL, translating to AUC/MIC ratios >100 for the pathogens listed above-well above the threshold.
Clinical Dosing and Practical Considerations
Standard regimens are:
- Acute bacterial conjunctivitis: one drop in each eye twice daily for 5days.
- Keratitis (moderate‑to‑severe): one drop every 12hours, sometimes intensified to every 8hours for the first 24hours.
Because systemic exposure is trivial, dose adjustments for renal or hepatic impairment are unnecessary. However, consider the following:
- Contact lens wearers: remove lenses before instillation and wait 15minutes before reinserting.
- Dry eye patients: the viscous formulation may cause transient blur; advise patients to keep eyes closed for ~1minute after dosing.
- Allergy history: although preservative‑free, rare hypersensitivity reactions have been reported; discontinue if redness worsens.
Comparative PK/PD Snapshot
| Parameter | Besifloxacin | Moxifloxacin | Gatifloxacin |
|---|---|---|---|
| Cmax (aqueous, µg/mL) | 1.5 | 0.9 | 0.8 |
| Tmax (hours) | 0.5 | 0.8 | 1.0 |
| Half‑life (hours) | 3.2 | 2.5 | 2.8 |
| Protein binding (tear fluid) | ~10% | ~15% | ~12% |
| AUC (µg·h/mL) | 12 | 7 | 6.5 |
| PK/PD Index (AUC/MIC) for S. aureus | >120 | >70 | >60 |
Besifloxacin’s higher Cmax and prolonged half‑life give it a comfortable PK/PD buffer, especially against resistant strains.

Quick Checklist for Practitioners
- Confirm diagnosis of bacterial conjunctivitis or keratitis before prescribing.
- Use the standard twice‑daily dosing; consider an 8‑hour interval for severe keratitis.
- Educate patients on proper drop technique and the need to keep eyes closed briefly.
- Monitor for ocular irritation or rare hypersensitivity; discontinue if needed.
- Remember: No systemic dose adjustment required, even in renal/hepatic impairment.
Future Directions and Research Gaps
While besifloxacin’s ocular PK is well‑characterized, a few areas need more data:
- Posterior segment penetration: Limited studies on vitreous concentrations; could inform off‑label uses.
- Long‑term resistance trends: Surveillance in community‑acquired conjunctivitis is sparse.
- Combination therapy: Potential synergy with anti‑inflammatory agents for severe keratitis.
Ongoing pharmacometric modeling aims to refine dosing for pediatric patients, where corneal thickness and tear turnover differ from adults.
Frequently Asked Questions
How quickly does besifloxacin reach therapeutic levels in the eye?
Therapeutic concentrations are typically observed within 30minutes after a single drop, with peak levels (Cmax) around 1.5µg/mL in the aqueous humor.
Is systemic exposure a concern with besifloxacin?
No. Systemic absorption is negligible (<0.1% of the administered dose), so drug‑drug interactions and systemic side‑effects are essentially absent.
Can besifloxacin be used for viral conjunctivitis?
No. Besifloxacin targets bacterial DNA gyrase; it has no activity against viruses. Use antiviral agents or supportive care for viral cases.
What makes besifloxacin more effective than older fluoroquinolones?
Its higher corneal penetration, lower protein binding, and dual‑target inhibition (DNA gyrase & topoisomeraseIV) produce higher intra‑ocular concentrations and a wider PK/PD margin, especially against resistant strains.
Are there any special storage requirements?
Store the suspension at room temperature, protected from light. Do not freeze. Once opened, use within 30days to maintain potency.

 Pharmacology
Pharmacology
Jacob Miller
October 1, 2025 AT 18:39Looks like someone tried to make a fancy calculator but forgot the basics. The Cmax/MIC logic is oversimplified, especially when you consider tear turnover. If you’re going to publish this, at least double‑check the if condition – it’s broken. Anyway, good luck convincing anyone with this half‑baked math.
Anshul Gandhi
October 12, 2025 AT 04:39First off, the whole premise that a single ocular drop can be reduced to a binary effective/marginal output is naïve. You’re ignoring the pharmacodynamic nuances that have been documented since the 1990s. Moreover, the hidden JavaScript condition `if (isNaN(micValue) || micValue = 8)` is a blatant typo that flips the logic. Anyone with a clue knows that `=` assigns, not compares, so the calculator will always flag “Effective” regardless of the input. This is not a harmless slip; it’s an intentional manipulation to make the drug look better. Don’t be surprised if the same code appears in other “official” pharma tools – it’s part of a larger data‑shaping agenda. The pharmaceutical lobby has been known to seed such scripts into open‑source repositories to steer prescribing patterns. They rely on clinicians not noticing the subtle bugs and then prescribing the product en masse. The Cmax of 1.5 µg/mL is quoted without any reference to inter‑patient variability. Tear turnover rates can differ by a factor of three, which directly impacts the achieved MIC ratio. If you factor in those variations, many strains will fall below the eight‑fold threshold. Yet the calculator pretends a one‑size‑fits‑all scenario, which is dangerous. Clinicians should cross‑check with validated PK/PD models instead of trusting this black‑box widget. In short, the tool is a marketing veneer, not a scientific decision aid. Proceed with caution and demand transparent code before integrating it into practice.
Emily Wang
October 22, 2025 AT 14:39Great effort pulling together the PK data! The 30‑minute Tmax aligns nicely with what we see in clinical trials. Remember to highlight that protein binding in tears is low, which boosts free drug levels. Also, the half‑life of roughly 4‑5 hours gives you flexibility for BID dosing. Keep the checklist – it’s exactly the kind of quick reference busy clinicians love.
Emma French
November 1, 2025 AT 23:39The PK/PD ratio threshold of eight is a solid benchmark for fluoroquinolones.
Debra Cine
November 12, 2025 AT 09:39Loved the clear breakdown – super helpful! 👍 The emoji vibe makes the science feel more approachable. Keep the friendly tone, it really encourages discussion.
Rajinder Singh
November 22, 2025 AT 19:39Behold the saga of a droplet’s journey!
From the rim of the eye it slides, daring to breach the corneal barrier with the poise of a seasoned protagonist. Its lipophilic charm (logP≈2.1) grants it passage, yet its aqueous disguise ensures clarity. The drama culminates in a Cmax of 1.5 µg/mL, a climax worthy of applause. Such a performance deserves a standing ovation in any ophthalmic theater.
Taylor Van Wie
December 3, 2025 AT 05:39This drug is proudly American-made and should stay in American hands.
Any foreign competition is just a distraction.
carlee Lee
December 13, 2025 AT 15:39Solid data, concise presentation.
Will reference in my notes.
chuck thomas
December 24, 2025 AT 01:39Pharmacokinetics is the bridge between chemistry and patient outcomes; crossing it thoughtfully yields better care.
When we honor the math, we honor the patient.
Let’s keep questioning the numbers.
Gareth Pugh
January 3, 2026 AT 11:39Besifloxacin’s ocular journey is a symphony of diffusion and kinetics.
Each note, from Cmax to half‑life, orchestrates therapeutic harmony.
Illiana Durbin
January 13, 2026 AT 21:39For anyone starting out, remember to verify the MIC value before trusting the ratio.
Eye drop technique matters – a quick blink can improve drug retention.
These small steps can shift the Cmax/MIC balance in your favor.
Tyler Heafner
January 24, 2026 AT 07:39It is advisable to consult the latest clinical guidelines when interpreting PK/PD ratios.
Adherence to established protocols ensures optimal therapeutic outcomes.
Michael Daun
February 3, 2026 AT 17:39nice breakdown but watch ur spelling tehre
also, less punctuation makes it easier to read