For many people with gout, the pain comes and goes - but the real problem isn’t just the flare-ups. It’s the invisible buildup of urate crystals in your joints, slowly damaging tissue over years. That’s why modern gout care doesn’t stop at pain relief. The goal now is simple: get your serum urate level below 6 mg/dL and keep it there. This isn’t just a number on a lab report. It’s the threshold that stops new crystals from forming and starts dissolving the old ones. And two drugs - allopurinol and febuxostat - are at the heart of making this happen.
Why 6 mg/dL? The Science Behind the Target
Urate, or uric acid, is a waste product your body makes when breaking down purines. When levels stay too high, it crystallizes in your joints. That’s gout. But here’s the key: at 6.8 mg/dL, urate starts to crystallize. So why aim for 6 mg/dL and not just under 6.8? Because science shows you need to go below saturation to dissolve existing crystals. Studies tracking people over years found that keeping urate below 6 mg/dL cuts flare frequency by 74%. For those with tophi (those visible lumps under the skin), the target drops even lower - to 5 mg/dL. At that level, tophi shrink by nearly 90% over 12 to 18 months.
This isn’t guesswork. It’s based on data from over 3,800 patients in randomized trials and decades of real-world outcomes. The 2020 American College of Rheumatology guidelines made this official: if you have gout and need treatment, your urate should be below 6 mg/dL. No exceptions. Even if you haven’t had a flare in a year, if crystals are still there, you’re at risk. And if you’ve got tophi or joint damage? You need to get even lower - below 5 mg/dL. But don’t go too low. Below 3 mg/dL, there’s no added benefit, and it might even cause problems.
Allopurinol: The First-Line Workhorse
Allopurinol has been the go-to drug for gout since the 1960s. It works by blocking xanthine oxidase, the enzyme that makes uric acid. It’s cheap - often less than $10 a month - and works well. But here’s the catch: most people don’t get enough of it.
Doctors often start with 100 mg a day. That’s too low for most adults. In real life, 30 to 50% of patients need doses of 400 mg or more to reach target levels. Some even need 600 to 800 mg daily. And yes, that’s safe if your kidneys are okay. The trick? Don’t start high. Start low - especially if you have kidney disease - and increase slowly. Every 2 to 4 weeks, check your urate level. If it’s still above 6 mg/dL, bump the dose up by 50 to 100 mg. Most people need 6 months or longer to get there.
There’s one big safety concern: allopurinol hypersensitivity syndrome. It’s rare - less than 0.4% of people - but it can be deadly. The risk jumps 25 times if you carry the HLA-B*5801 gene. That’s why some places now test for it before starting, especially in people of Asian descent. If you’ve ever had a severe rash or liver problems on allopurinol, don’t take it again.
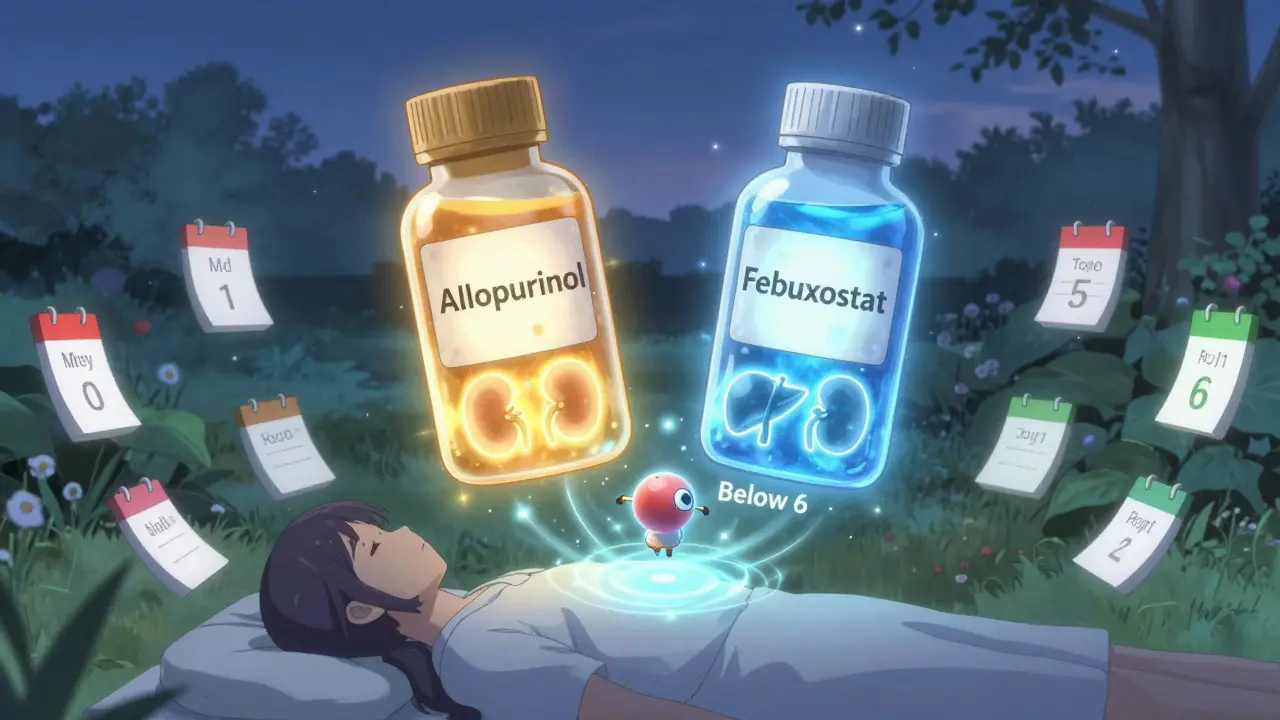
Febuxostat: The Alternative for Tough Cases
Febuxostat does the same job as allopurinol - blocks uric acid production - but it’s not processed by the kidneys the same way. That makes it a better option if you have moderate to severe kidney disease. A 2023 meta-analysis found febuxostat helped 15% more patients hit their target than allopurinol in those with CKD stage 3 or worse.
It’s also more potent. Most people start at 40 mg a day and can go up to 80 mg if needed. It often gets people to target faster than allopurinol. But it’s more expensive - $30 to $50 a month in the U.S. - and has a black box warning for possible heart-related risks. That doesn’t mean you can’t use it. It means you need to be careful if you have heart disease. If you’re at risk for heart attack or stroke, your doctor might stick with allopurinol.
Who Gets Which Drug? The Real-World Choice
Guidelines don’t always agree. The American College of Rheumatology says allopurinol should be first for everyone. The European League Against Rheumatism says the same - unless you have kidney problems. The UK’s NICE guidelines say either is fine, depending on cost, kidney function, and patient preference.
In practice, most people start with allopurinol. Why? Cost. Availability. Familiarity. But if you’ve tried allopurinol and can’t get your urate down even at 600 mg, or if you had a bad reaction - febuxostat becomes your next step. It’s not better for everyone. But for some, it’s the only thing that works.
And here’s something most patients don’t know: if you’re on either drug and still getting flares, it doesn’t mean the drug isn’t working. It might mean your body is dissolving crystals - and that can trigger inflammation. This is called the "flare paradox." It’s temporary. Keep taking the medicine. Your doctor might add a low-dose colchicine or NSAID for a few months to help you through this phase.

Why Most People Fail - And How to Succeed
Only about 42% of gout patients reach their target urate level within a year. Why? Three big reasons:
- Underdosing: Doctors start too low and don’t titrate up. A 2023 study found 68% of dose failures were because the patient never got past 300 mg of allopurinol.
- Missing tests: You can’t manage what you don’t measure. Only 54% of patients on ULT get their urate checked monthly during titration, as recommended.
- Stopping too soon: Many quit because they feel fine. But crystals don’t vanish overnight. It takes 6 to 18 months to dissolve them. If you stop, they come back.
Success comes from three things: regular blood tests, patience, and persistence. Get your urate checked every 2 to 4 weeks while adjusting your dose. Once you hit target, check every 6 months. Stick with the medicine even when you feel fine. And if you’re not reaching target, don’t assume it’s your fault. Talk to your doctor about higher doses or switching drugs.
What’s Next? Precision Dosing and New Tools
The future of gout treatment is getting smarter. In 2024, the GOUT-PRO study showed that testing for certain gene variants (ABCG2 and SLC22A12) before starting allopurinol increased the chance of reaching target from 61% to 83%. These genes affect how your body processes the drug. If you’re a slow metabolizer, you need a lower dose. If you’re a fast one, you need more.
Also, new drugs are coming. Verinurad, a uricosuric that helps your kidneys excrete more uric acid, is in late-stage trials. It may work better with allopurinol than either drug alone. And by 2025, results from the ULTRA-GOUT trial will tell us if a fixed-dose approach works as well as the current “treat-to-target” method.
For now, the message is clear: gout is not just about pain. It’s about chemistry. And with the right drug, the right dose, and regular monitoring, you can beat it.
What is the target serum urate level for gout?
The standard target for all gout patients on urate-lowering therapy is below 6 mg/dL (360 micromol/L). For those with tophi, chronic joint damage, or frequent flares, the target drops to below 5 mg/dL (300 micromol/L). These levels are based on guidelines from the American College of Rheumatology, NICE, and EULAR. Going below 3 mg/dL is not recommended because there’s no added benefit and potential risks.
Is allopurinol or febuxostat better for gout?
Allopurinol is usually the first choice because it’s cheaper and effective for most people. Febuxostat is preferred if you have moderate to severe kidney disease or can’t tolerate allopurinol. Studies show febuxostat helps 15% more patients reach target levels in advanced kidney disease. However, febuxostat has a black box warning for heart risks, so it’s not ideal if you have heart disease. The best choice depends on your kidney function, cost, and past reactions.
Why do I still get flares after starting allopurinol?
This is called the "flare paradox." When urate-lowering therapy starts, crystals begin to dissolve, and that can trigger inflammation. It’s not a sign the drug isn’t working - it’s a sign it is. Most doctors recommend taking a low dose of colchicine or an NSAID for the first 3 to 6 months to prevent these flares. Keep taking your allopurinol. The flares usually stop once your urate level stays below 6 mg/dL for a few months.
How long does it take to dissolve gout crystals?
It takes time. Even with perfect dosing, it can take 6 to 18 months to dissolve existing urate crystals. That’s why you need to stay on your medication even if you haven’t had a flare in a year. Stopping too early lets crystals rebuild. Your doctor may use imaging like dual-energy CT to confirm crystal dissolution before considering stopping treatment.
Do I need to get my urate level tested regularly?
Yes - and often. During the first 6 to 12 months, your urate level should be checked every 2 to 4 weeks while your dose is being adjusted. Once you hit target, check every 6 months. Studies show that patients who get monthly testing during titration are 31% more likely to reach their target than those checked only quarterly. If you’re not getting tested regularly, ask your doctor why.

 Pharmacology
Pharmacology