Facial flushing isn’t just blushing after a spicy meal or a stressful meeting. For millions of people, it’s the first sign of something deeper-rosacea. This isn’t acne. It’s not just dry skin. It’s a chronic condition that turns your face into a map of redness, heat, and sometimes bumps that won’t go away. And if you’ve been told it’s just sensitivity, you’re not alone. But the truth is, rosacea has a name, a pattern, and real treatment options-especially when it comes to topical antibiotics.
What Rosacea Really Looks Like
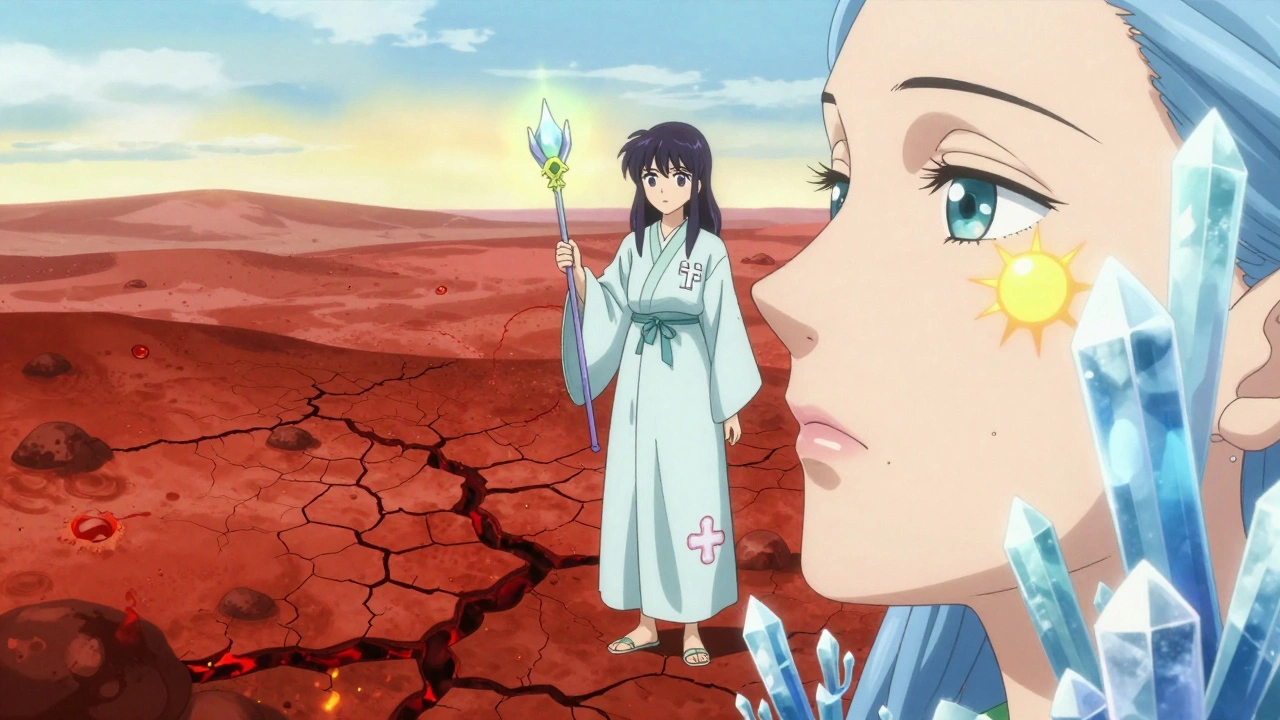
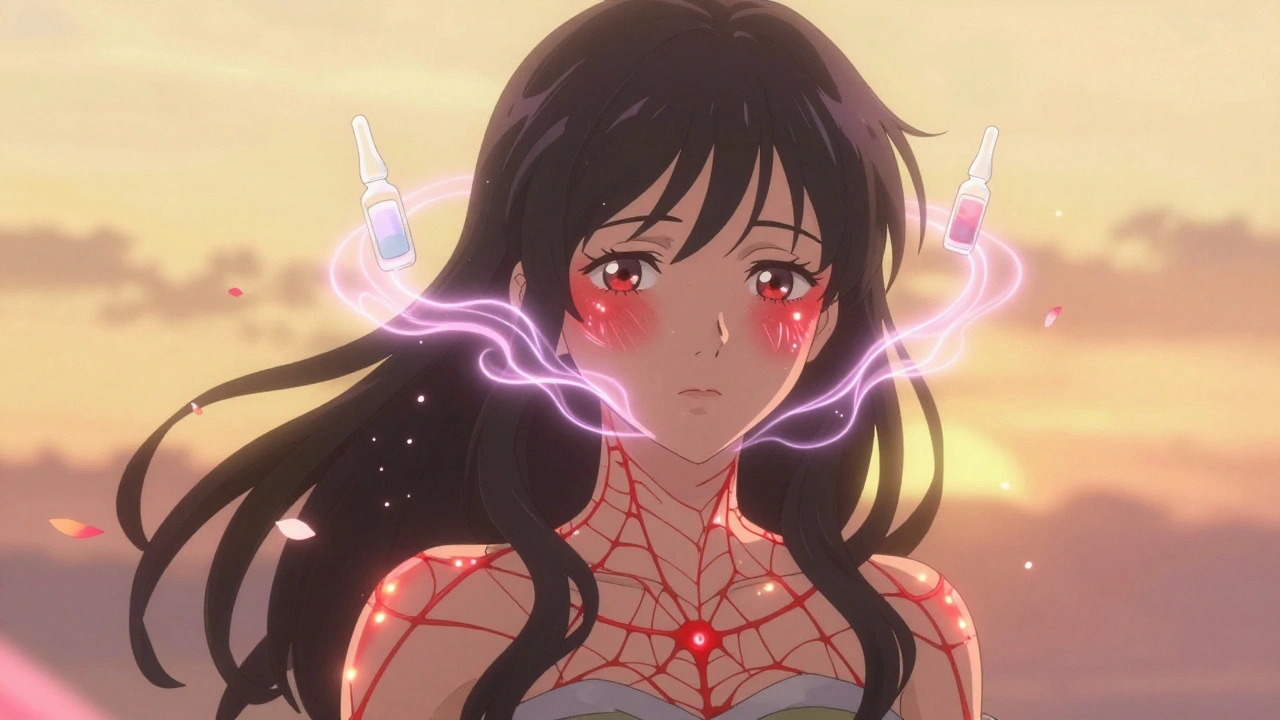
Rosacea doesn’t show up overnight. It creeps in. Maybe you notice your cheeks get red after coffee. Or your forehead stays flushed long after you’ve cooled down. That’s not normal blushing. Normal blushing fades in minutes. Rosacea flushing lasts hours. It’s triggered by heat, alcohol, spicy food, sun, even stress. And once it starts, it doesn’t just go back to normal. Over time, the redness becomes permanent. That’s called persistent erythema. It’s not a sunburn you can wash off. It’s a deep, lasting redness that covers your nose, cheeks, chin, and forehead.Up to 75% of people with rosacea start with flushing. By the time they see a dermatologist, many already have visible blood vessels-tiny red lines that look like spiderwebs under the skin. Around half of those people develop papules and pustules-small red bumps or pus-filled spots that mimic acne. But unlike acne, there’s no blackhead. No oil. Just inflammation. And for about half of all rosacea patients, their eyes get involved too: dryness, burning, light sensitivity. It’s not just a skin issue. It’s a whole-body experience.
Why Topical Antibiotics? It’s Not About Bacteria
You might wonder: why use antibiotics on your face if it’s not an infection? That’s the big misconception. Rosacea isn’t caused by bacteria like acne is. But here’s the twist: the same drugs that kill bacteria also calm inflammation. That’s why metronidazole, ivermectin, and azelaic acid work-even though they don’t all fight germs.Metronidazole has been around since the 1980s. It’s cheap, widely available, and gentle. It reduces red bumps and pustules by about 60-70% after 6-9 weeks. But it doesn’t touch the flushing. It doesn’t fade the redness. It just calms the bumps.
Ivermectin, approved in 2014, changed the game. In a 2019 study of 900 patients, 76% saw their bumps cut in half after 12 weeks. That’s better than metronidazole. Why? Because ivermectin doesn’t just fight inflammation-it targets Demodex mites. These microscopic bugs live on everyone’s skin. But in rosacea, they multiply. And their waste triggers an immune reaction. Ivermectin kills them. No more mite mess. Less inflammation. Fewer bumps.
Azelaic acid is different. It’s not an antibiotic. But it’s just as effective. It reduces bumps by 68-73% over 15 weeks. It works by calming the skin’s immune response and reducing excess pigment. It’s great for people who get post-inflammatory red marks after bumps heal.
What the Experts Say
Dermatologists don’t treat rosacea like a one-size-fits-all problem. Dr. Linda Stein Gold, a leading expert, says ivermectin is now the go-to for papulopustular rosacea. Why? Because it hits two targets: inflammation and mites. But Dr. Hilary Franck reminds us: antibiotics alone aren’t enough. You can’t just slap on cream and ignore your triggers.That’s the key. Topical antibiotics treat the bumps. They don’t fix the flushing. For that, you need other tools-like brimonidine or oxymetazoline gels that shrink blood vessels temporarily. But those are for short-term relief. Antibiotics are for long-term control.
And here’s the hard truth: most people quit. Studies show only 40-50% stick with topical treatment past three months. Why? Because results take time. You won’t see a difference in three days. It takes four to eight weeks just to start noticing. And in the first two weeks? Your skin might get worse. Burning. Flaking. Redder than ever. That’s not the treatment failing. It’s your skin adjusting. If you quit then, you’ll never know what it could’ve done.

How to Use These Treatments Right
Using these creams wrong is like taking a painkiller and then eating spicy food. You’re fighting yourself.- Use a pea-sized amount for your whole face. Too much just irritates.
- Apply to completely dry skin. Wait 15 minutes after washing.
- Don’t layer it over other actives like retinoids or acids. That’s asking for irritation.
- Use sunscreen every day. Mineral sunscreen with zinc oxide is best. Chemical sunscreens can sting.
- Start slow. If you’re new to this, patch-test on your jawline for three days before going full-face.
Some people find applying the cream to slightly damp skin helps reduce stinging. Others switch to the 0.75% version of metronidazole instead of the stronger 1% to ease into it. And always pair it with a gentle, fragrance-free moisturizer. Ceramides help rebuild your skin barrier so it doesn’t get so reactive.
Real People, Real Results
On Reddit’s r/Rosacea, users share their wins and struggles. One person wrote: “After 8 weeks of ivermectin, my bumps were down 80%. No more hiding behind makeup.” Another said: “Metronidazole made my face look like a burn for two weeks. I almost quit. But then it cleared up. Best decision I ever made.”But it’s not all good news. About 16% of users on Drugs.com say it didn’t help. Some say it’s too expensive-up to $350 a year without insurance. Others say the side effects aren’t worth it. And that’s valid. Not everyone responds. But for the majority, the trade-off is worth it.
What Doesn’t Work
Don’t expect topical antibiotics to fix flushing. They won’t. Don’t use harsh scrubs, alcohol-based toners, or essential oils. They’ll make it worse. And don’t assume you can stop once you feel better. Rosacea is chronic. Stopping treatment often means symptoms come back-sometimes worse.Also, don’t rely on “natural” cures. Aloe vera, tea tree oil, coconut oil-these might soothe temporarily, but they don’t change the underlying inflammation. And some, like tea tree oil, can actually trigger flare-ups.
When to See a Dermatologist
If your face stays red for more than a few days, if you get bumps that don’t pop, if your eyes feel gritty or sore, or if your skin feels like it’s on fire after a warm shower-it’s time to see a specialist. General practitioners rarely have the tools or experience to manage rosacea properly. Dermatologists know which triggers to look for, which creams to prescribe, and when to add other treatments.And if you’ve tried topical antibiotics for 8 weeks and seen less than 25% improvement? It’s time to switch. Maybe you need ivermectin instead of metronidazole. Or maybe you need azelaic acid. Or a combination. Your dermatologist can help you adjust.
The Bigger Picture
The global rosacea treatment market is growing fast-projected to hit $2.7 billion by 2030. Why? Because more people are being diagnosed. And more people are finding relief. Topical antibiotics aren’t magic. But they’re the most reliable tool we have for controlling the bumps and inflammation that make rosacea so hard to live with.What’s coming next? New combinations. Like ivermectin mixed with hydrocortisone. Early trials show 85% reduction in bumps-better than either alone. That’s the future: smarter, multi-targeted treatments.
But right now? The best thing you can do is start. Be patient. Be consistent. Protect your skin. And don’t let the redness win.
Can topical antibiotics cure rosacea?
No, topical antibiotics don’t cure rosacea. Rosacea is a chronic condition with no known cure. But these treatments can significantly reduce symptoms like red bumps and pustules. With consistent use, many people achieve long-term control and clear skin, but stopping treatment usually leads to a return of symptoms.
Why does my skin get worse before it gets better with topical antibiotics?
It’s common for rosacea treatments to cause temporary irritation, especially in the first 1-2 weeks. This happens because your skin is adjusting to the new product. Metronidazole and ivermectin can cause stinging, dryness, or increased redness initially. This doesn’t mean the treatment isn’t working-it’s often a sign your skin is reacting before calming down. Stick with it unless the irritation becomes severe.
Do I need to use sunscreen if I’m using topical antibiotics?
Yes, absolutely. Sun exposure is one of the top triggers for rosacea flushing and inflammation. Topical antibiotics don’t protect your skin from UV damage. Use a mineral sunscreen with zinc oxide (10-20%) every day, even when it’s cloudy. Chemical sunscreens can irritate sensitive rosacea-prone skin, so avoid them.
Is ivermectin better than metronidazole for rosacea?
Yes, in most cases. A 2019 study showed ivermectin reduced inflammatory lesions by 76% compared to 55% with metronidazole. Ivermectin also targets Demodex mites, which play a role in rosacea inflammation. However, metronidazole is gentler and often recommended for people with very sensitive skin or those trying treatment for the first time.
How long until I see results from topical antibiotics?
Most people start noticing improvement after 4-6 weeks, but full results take 12-16 weeks. Don’t expect overnight changes. Rosacea develops over months or years, and so does its improvement. Consistency matters more than speed. If you don’t see at least 25% improvement after 8 weeks, talk to your dermatologist about switching treatments.
Can I use makeup with topical antibiotics?
Yes, but wait at least 15 minutes after applying the medication before putting on makeup. Use non-comedogenic, fragrance-free products. Mineral-based foundations with zinc oxide can even help soothe the skin and provide extra sun protection. Avoid heavy, oil-based formulas-they can clog pores and worsen inflammation.
 Pharmacology
Pharmacology
David Brooks
December 6, 2025 AT 15:14OMG I finally got my rosacea under control after 7 years of suffering. Ivermectin was a GAME CHANGER. My face doesn’t look like a tomato anymore. I used to hide behind scarves in summer. Now I wear tank tops. Tears. Just tears. Thank you for this post.
Helen Maples
December 8, 2025 AT 05:52You're wrong to say topical antibiotics don't treat flushing. They reduce the inflammatory cascade that exacerbates vasodilation. The redness isn't just vascular-it's neurogenic inflammation amplified by Demodex. Ivermectin works because it modulates TLR2 and cathelicidin pathways. Stop oversimplifying.
Jane Quitain
December 8, 2025 AT 18:36i just started metronidazole last week and my face is on FIRE 😭 but i’m sticking with it bc everyone says it gets better. pray for me 🙏
Ted Rosenwasser
December 9, 2025 AT 18:20Let me be the first to point out the glaring flaw in this ‘evidence-based’ piece: you cite a 2019 study but ignore the 2022 meta-analysis from the Journal of the American Academy of Dermatology that found no statistically significant difference between ivermectin and azelaic acid in long-term remission rates. Also, Demodex mites are ubiquitous-calling them the ‘cause’ is pseudoscience dressed up as medicine. You’re selling a narrative, not data.
And don’t get me started on the ‘natural remedies’ bashing. Aloe vera has anti-inflammatory cytokines. Coconut oil has lauric acid. You’re dismissing centuries of ethnopharmacology because it doesn’t fit Big Pharma’s patent timeline.
Also, why is the global market projected to hit $2.7B? Because they’ve turned a chronic condition into a lifelong revenue stream. You’re not helping-you’re monetizing insecurity.
And yes, I’ve read the papers. And no, I’m not a dermatologist. But I am someone who reads beyond the abstract.
Kyle Oksten
December 10, 2025 AT 01:07There’s a deeper truth here: we treat rosacea like a bug to be eradicated, not a signal from our bodies. The flushing? It’s not random. It’s your nervous system screaming that something’s off-diet, stress, gut dysbiosis, even circadian disruption. Antibiotics silence the symptom, not the cause. We’ve built a whole industry around suppressing the messenger while ignoring the message.
Maybe the real breakthrough isn’t a new cream-it’s learning to listen to your skin again. What if your rosacea isn’t a disease to cure… but a teacher to understand?
Louis Llaine
December 10, 2025 AT 11:58So you spent 1200 words telling people to use sunscreen and not to eat spicy food. Groundbreaking. I didn’t know my face was a sensitive snowflake. Next you’ll tell me not to breathe.
Nicholas Heer
December 11, 2025 AT 10:31They don’t want you to know this but the FDA approved ivermectin for rosacea because the pharmaceutical lobby bought off the review board. The real cause? 5G radiation + glyphosate in your water. The mites? A distraction. They want you dependent on creams so you never ask why your town’s water supply is laced with neurotoxins. Wake up. This isn’t medicine-it’s control.
Sadie Nastor
December 12, 2025 AT 13:10my skin broke out so bad the first week i cried and almost quit… but i kept going and now it’s the best it’s been in 5 years 🥹 thank you for not sugarcoating how hard it is at first 💪
Olivia Hand
December 14, 2025 AT 00:49Has anyone tried combining azelaic acid with low-dose oral doxycycline? I’ve seen a few case studies where the combo reduced flushing by 40% more than topical alone. Not saying it’s for everyone-but maybe the real answer isn’t just one cream. Maybe it’s layered, personalized. We treat acne like a puzzle. Why not rosacea?
Sam Mathew Cheriyan
December 14, 2025 AT 16:36bro i tried ivermectin and it made my face look like i got sunburnt in the sahara… then i switched to turmeric paste and my skin cleared in 3 days. the truth is they dont want you to know about natural cures. its all about the money man.
Ernie Blevins
December 15, 2025 AT 06:18lol you think this works? I’ve been on 3 different creams. My face looks like a crime scene. I’m just waiting for the day I can’t leave the house.
Nancy Carlsen
December 16, 2025 AT 00:37to anyone just starting out: you’re not broken. you’re not ugly. you’re not alone. this is hard, but you’re stronger than the redness. i’m cheering for you. 💕
Oliver Damon
December 17, 2025 AT 22:46There’s a fascinating paradox here: we use anti-inflammatories to treat inflammation, yet we rarely address the root drivers-sleep deprivation, chronic stress, gut permeability. The skin is a mirror. Rosacea isn’t just a dermal condition; it’s a systemic stress response. Topical agents are palliative. Real healing requires lifestyle recalibration. We’re treating the symptom because we’re afraid of the cause.
And yet, the fact that ivermectin reduces Demodex populations so effectively suggests the immune system is already primed for dysregulation. Maybe the real question isn’t ‘what cream works?’ but ‘why is our microbiome collapsing?’
Ashley Farmer
December 19, 2025 AT 04:42Thank you for writing this. I’ve been too afraid to talk about my rosacea because I thought people would think I was just ‘red-faced’ or ‘overreacting.’ This helped me feel seen. I’m starting ivermectin next week. I’ll update you if it works. You’re not alone.