It’s easy to think taking a little extra help for a cold or headache is harmless. But if you’re already on prescription meds, that extra pill could be dangerous - not because of what it does, but because of what it doubles.
Why Double Ingredients Are More Dangerous Than You Think
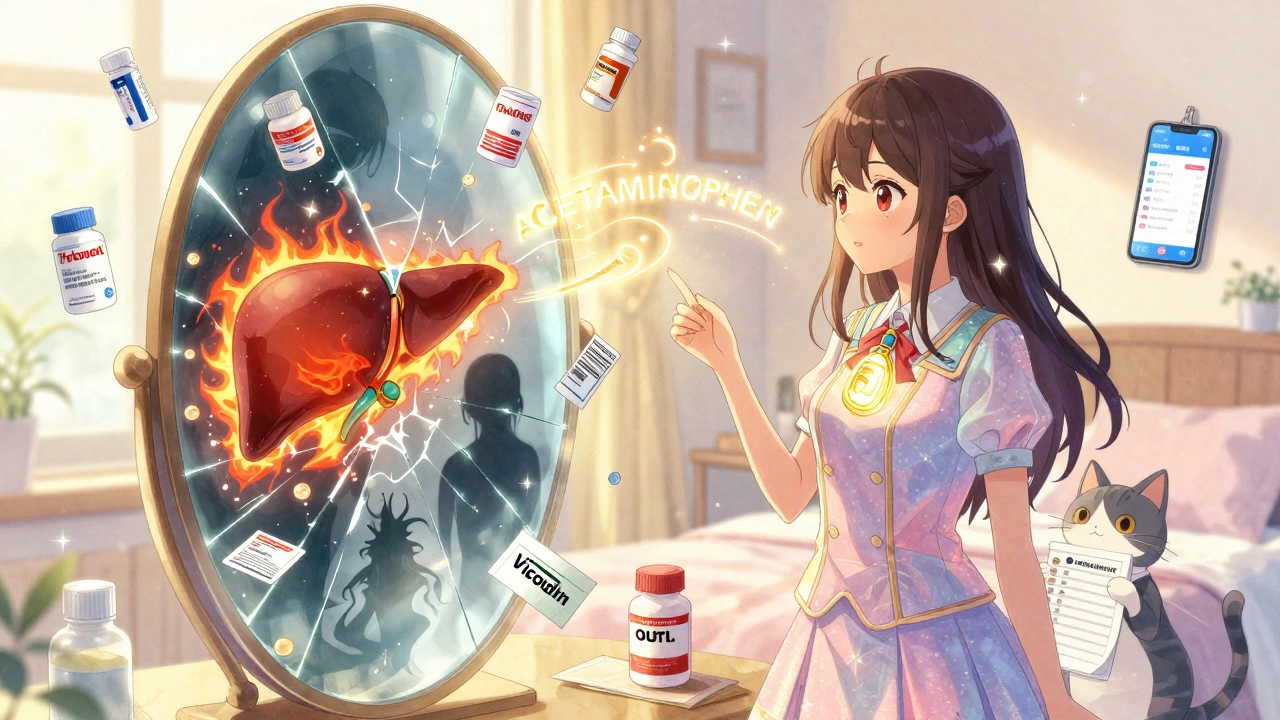
You might not realize it, but many common over-the-counter (OTC) medicines share the same active ingredients as your prescriptions. Acetaminophen, for example, is in more than 600 products - from painkillers like Vicodin to cold syrups, sleep aids, and even allergy pills. Taking two of these at once? You’re not doubling your relief. You’re risking liver failure. The CDC says adults over 65 make up 65% of hospital visits from accidental acetaminophen overdose. That’s not because they’re careless. It’s because they didn’t know. One pill says "Tylenol," another says "NyQuil," and a third is labeled "Hydrocodone/APAP." None of them scream "same drug inside." This isn’t just about painkillers. Sedatives like diphenhydramine (found in Benadryl and many sleep aids) mix dangerously with prescription anxiety or sleep meds. Pseudoephedrine in cold remedies can spike blood pressure when taken with certain heart or blood pressure pills. NSAIDs like ibuprofen can cause internal bleeding if you’re already on blood thinners - and you might not even know you’re taking two of them.Who’s at Highest Risk?
People taking five or more medications - what doctors call polypharmacy - are the most vulnerable. About 40% of older adults in the U.S. fall into this group. And it’s getting worse. Since 2010, the number of people with multiple chronic conditions has jumped 27%. More conditions mean more prescriptions. More prescriptions mean more chances for overlap. The problem isn’t just with prescriptions. Nearly half of all double ingredient errors happen when people take multiple OTC products at once. A 2022 MedlinePlus survey found that 61% of adults have had symptoms from hidden ingredient overlap - dizziness, extreme sleepiness, stomach bleeding, or confusion. And in 73% of those cases, it was cold or allergy meds doing the damage. Seniors are especially at risk because they often see multiple doctors - a cardiologist, a rheumatologist, a neurologist - and none of them ask about the OTC meds they’re taking. A 2021 study in the Journal of the American Geriatrics Society found that 67% of older adults who had double ingredient incidents said their doctors never asked about their non-prescription pills.How It Happens: The Hidden Traps
Most people don’t think of their cold medicine as a drug that interacts with their heart pill. They think of it as something you grab off the shelf. But here’s the reality: 45% of prescription labels don’t clearly warn you about ingredients that also appear in OTC products. And even when they do, the language is vague. "Contains acetaminophen" might be printed in tiny font next to a list of inactive ingredients. Another big trap? Using multiple pharmacies. If you get your blood pressure medicine from one store and your sleep aid from another, neither pharmacy’s system sees the full picture. A 2021 study in JAMA Internal Medicine found that using just one pharmacy cuts double ingredient errors by 63%. Why? Because pharmacists can see everything you’re taking - and their software flags duplicates. Even worse, 68% of people don’t tell their doctors about herbal supplements, vitamins, or traditional remedies. That’s a blind spot. A ginkgo biloba supplement might seem harmless - until it’s mixed with warfarin and causes internal bleeding. Or a turmeric pill that thins your blood, taken with aspirin. These aren’t rare cases. They’re predictable.What You Can Do Right Now
The good news? Almost 9 out of 10 of these errors are preventable - if you take simple steps.- Make a full list - every single thing you take. Prescription, OTC, vitamins, supplements, even herbal teas. Write down the name, dose, and how often you take it. Include the reason - for example, "ibuprofen 200 mg, 1 tablet daily for arthritis." Keep a copy in your wallet and another at home.
- Use one pharmacy - all your meds, all the time. Even if it’s less convenient. Your pharmacist becomes your safety net. They’ll catch duplicates before you even leave the store.
- Ask every provider - at every visit. Say: "Here’s my full list. Are any of these overlapping?" Don’t assume they’ve seen your other prescriptions. Bring the list. Read it out loud. Make them look at it.
- Check labels before buying OTC - don’t just grab the brand you remember. Look at the "Active Ingredients" section on the Drug Facts label. If you see acetaminophen, diphenhydramine, or ibuprofen, compare it to your list. If it’s already on there, don’t take it.
- Review once a year - with your primary doctor or pharmacist. Go through every item on your list. Ask: "Do I still need this? Is there a safer option?"
What’s Changing to Help You
The system is catching up. Since 2020, the FDA has required all OTC products to use a standardized "Drug Facts" label. The active ingredient must be bolded and listed first. But a 2023 Government Accountability Office report found 41% of people still can’t spot duplicates on those labels - so don’t rely on it alone. Electronic health records now have "double ingredient check" tools built in. Epic and Cerner, the two biggest systems, flag potential overlaps in 92% of cases - but only if the OTC meds are entered. And most patients still don’t tell their doctors about them. Apple Health and other smartphone apps now include medication trackers that alert you if you’re adding a duplicate. The FDA partnered with Apple to make this part of iOS 17. But again - it only works if you enter your meds correctly. If you type "Tylenol" instead of "acetaminophen," it won’t catch it.
Real Stories, Real Consequences
One Reddit user, "MedSafety101," shared how they took three different cold medicines - each with pseudoephedrine - and ended up in the ER with dangerously high blood pressure. Another patient at UCLA Health developed liver damage after taking their prescription painkiller and a store-brand cold syrup - both with acetaminophen. Neither knew they were the same. These aren’t isolated incidents. They’re symptoms of a system that treats each condition in a vacuum - one doctor for the heart, another for the joints, another for sleep - without ever asking: "What’s the full picture?"Final Rule: When in Doubt, Don’t Take It
If you’re already on a prescription that contains an active ingredient - like acetaminophen, ibuprofen, or diphenhydramine - don’t take another product with the same ingredient unless your doctor or pharmacist says it’s safe. Your body doesn’t care if the pill is called "Advil" or "ibuprofen." It only reacts to the chemical. And if you’ve already hit the daily limit, adding more won’t help - it will hurt. The safest way to manage multiple meds isn’t about memorizing names. It’s about knowing what’s inside. Keep your list. Use one pharmacy. Ask questions. And never assume OTC means safe.What are double ingredients in medications?
Double ingredients happen when you take two or more medications that contain the same active chemical - like acetaminophen in both a prescription painkiller and an OTC cold remedy. This can lead to overdose, even if you follow the directions on each bottle, because the total amount adds up beyond safe limits.
What’s the most dangerous double ingredient combination?
Acetaminophen is the most common and dangerous. It’s found in over 600 products, including painkillers, cold medicines, and sleep aids. Taking too much can cause severe liver damage - sometimes without symptoms until it’s too late. The NIH reports 56,000 emergency room visits each year in the U.S. from accidental acetaminophen overdose.
Can I take OTC meds with my prescriptions?
Maybe - but never assume it’s safe. Always check the active ingredients on the OTC label and compare them to your prescription list. If there’s any overlap - like ibuprofen, diphenhydramine, or pseudoephedrine - talk to your pharmacist or doctor first. Even "natural" supplements can interact.
Why do doctors not catch this?
Most electronic health records don’t include OTC meds unless the patient reports them. Many doctors focus on one condition at a time and don’t ask about non-prescription drugs. A 2021 study found 67% of patients who had double ingredient issues said their providers never asked about OTC use.
How can a pharmacist help me avoid double ingredients?
Pharmacists can see all your prescriptions in one system and flag duplicates. If you fill all your meds at one pharmacy, their software will warn you if a new drug contains an ingredient you’re already taking. They also offer free medication reviews - ask for one at least once a year.
Should I use a medication tracker app?
Yes - but only if you enter everything accurately. Apps like Apple Health can alert you to duplicates, but they rely on correct input. Type "acetaminophen," not just "Tylenol." And always cross-check with your physical list and your pharmacist. Apps help, but they’re not foolproof.
What should I do if I think I’ve taken too much of an ingredient?
Call Poison Control at 1-800-222-1222 immediately - don’t wait for symptoms. For acetaminophen, liver damage can start within hours. For sedatives like diphenhydramine, breathing problems can develop quickly. If you’re dizzy, confused, nauseous, or have abdominal pain after taking multiple meds, seek help right away.
 Pharmacology
Pharmacology
Mark Curry
December 6, 2025 AT 04:36Been there. Took NyQuil for a cold and ended up with a liver alarm from my bloodwork. Turns out my painkiller had acetaminophen too. Never again. Just one pharmacy, one list, no excuses.
Simple. But so many forget.
sean whitfield
December 7, 2025 AT 17:16Of course the system’s broken. Big Pharma doesn’t want you knowing your Tylenol and your Vicodin are the same damn thing. They profit off confusion. You think this is about safety? Nah. It’s about profit margins and your ignorance.
They’ll sell you five different bottles with the same chemical and call it ‘choice.’
Ada Maklagina
December 7, 2025 AT 19:38My grandma took three cold meds at once and ended up in the ER. No one asked what she was taking. She thought ‘natural’ meant safe. She was wrong.
Just say no to multitasking with meds.
Katie Allan
December 8, 2025 AT 01:01This is the kind of post that saves lives. Seriously. If you’re on more than three meds, stop scrolling and make that list right now. One pharmacy. One list. One life.
Don’t wait for a crisis to start caring.
Krishan Patel
December 8, 2025 AT 08:37Let me be clear: if you’re using multiple pharmacies, you’re playing Russian roulette with your liver. This isn’t a suggestion. It’s a survival rule. The fact that people don’t get this is why America’s healthcare system is a joke.
Pharmacists aren’t just cashiers. They’re your last line of defense.
Stephanie Fiero
December 9, 2025 AT 15:43I just typed ‘advil’ into my apple health app and it flagged my blood thinner. Thank god i added it. I thought it was just for fitness. Turns out it’s a lifesaver. Use the damn app. Even if you’re bad at typing.
it saved me.
Michael Dioso
December 10, 2025 AT 00:44Everyone’s acting like this is new. Newsflash: doctors have been ignoring OTC meds for decades. And you think a label change is gonna fix it? Please. The real issue is lazy medicine. One specialist per organ. No one looks at the whole body. It’s not a system. It’s a buffet of neglect.
And don’t even get me started on supplements. Ginkgo biloba? That’s just herbal warfarin with a yoga vibe.
James Moore
December 11, 2025 AT 22:33Look, I’m an American, and I respect the Constitution-but I don’t respect the FDA’s half-assed labeling. They let companies bury active ingredients in tiny print like they’re hiding evidence. And then they act surprised when old folks overdose? That’s not negligence. That’s corporate malice. And the government lets it happen because Big Pharma donates to both parties. This isn’t a health crisis-it’s a political crime.
Who’s really behind this? Who profits when you go to the ER? Not you. Not your doctor. Them.
aditya dixit
December 12, 2025 AT 22:41One pharmacy. One list. One conversation. These aren’t tips. They’re the bare minimum.
I’ve seen patients in India do this with paper notebooks and no apps. If they can do it with no tech, we have no excuse.
Start today. Not tomorrow. Today.
Laura Saye
December 14, 2025 AT 09:50I used to think ‘natural’ meant harmless. Then I started taking turmeric for inflammation and my INR went wild. Turns out, it’s a mild anticoagulant. My pharmacist caught it. I cried. Not because I was scared-but because no one had ever asked me about the little brown pills in my drawer.
It’s not about being perfect. It’s about being seen.
Juliet Morgan
December 16, 2025 AT 07:22My mom took a sleep aid with her heart med. She didn’t know diphenhydramine was in both. She woke up confused, barely breathing. We almost lost her.
Now I print her meds on a card and carry it in her purse. It’s not fancy. But it works.
Lucy Kavanagh
December 17, 2025 AT 08:29Apple Health? Please. That’s just another way for Big Tech to sell your data. And don’t tell me ‘it’s free’-if you’re not paying, you’re the product. They’re tracking your meds so they can sell you targeted ads for ‘better sleep’ and ‘stronger immunity.’
Real safety? Paper list. One pharmacy. No apps. No trust. Just facts.
Chris Brown
December 17, 2025 AT 23:06People think they’re being responsible by reading labels. But the truth? Most can’t read. They see ‘acetaminophen’ and think ‘that’s not me.’ They don’t know APAP means the same thing. They don’t know NyQuil is poison with a smiley face.
And now we have a nation of people who think ‘OTC’ means ‘safe.’ That’s not ignorance. That’s a cultural failure.