Every year, over 51 million dispensing errors happen in U.S. pharmacies. Most of these mistakes never reach patients-not because of barcode scanners or double-check systems, but because a pharmacist asked a simple question: "What is this medication for?" That moment of conversation is the last, most powerful line of defense against a wrong dose, a mix-up, or a dangerous interaction. It’s not just good practice. It’s proven, life-saving work.
Why Counseling Catches What Machines Can’t
Barcode scanners catch about 53% of dispensing errors. Pharmacist double-checks catch 67%. But when a pharmacist talks to a patient, error detection jumps to 83%. Why? Because machines can scan a pill bottle. They can’t ask, "Do you remember taking this before?" or "Why did your doctor say to take this twice a day?" The real power of counseling is that it turns the patient into a safety partner. If someone says, "I’ve been taking this red pill for my heart, but this one’s white," that’s a red flag. No automated system would notice the color change unless it was programmed to recognize every possible variation. But a patient who’s paying attention? They’ll spot it.The Four Key Checks That Catch Errors
Effective counseling isn’t just chatting. It’s a structured verification process. According to the UConn School of Pharmacy and the American Pharmacists Association, every counseling session should include these four checks:- Confirm the purpose - Ask: "What condition are you taking this for?" Don’t assume. A patient might say "for blood pressure," but the script is for diabetes. This catches 38% of wrong-medication errors.
- Verify understanding - Use the teach-back method. Ask: "Can you show me how you’ll take this?" If they say "I crush it and mix it in juice," and the medication shouldn’t be crushed? That’s a mistake caught before it leaves the pharmacy.
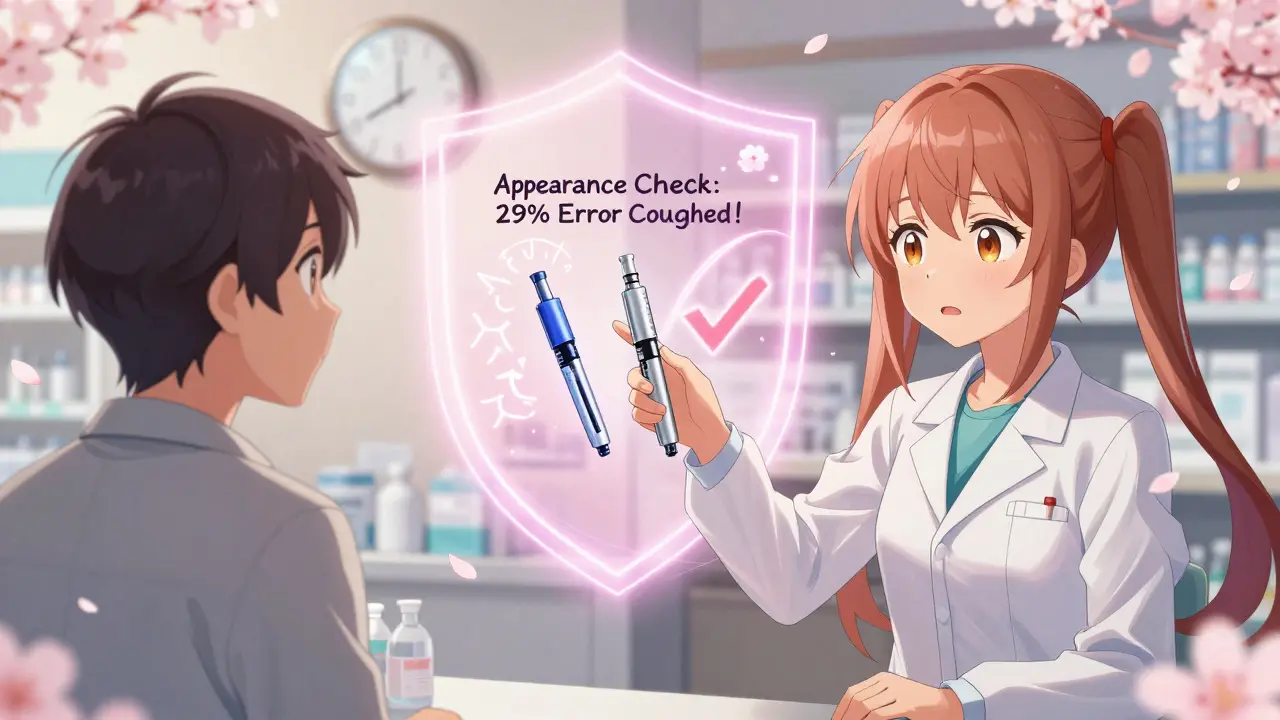
- Check the appearance - Show the patient the medication and ask: "Does this look like what you’ve taken before?" Look-alike drugs like insulin glargine and insulin lispro are mixed up all the time. This step alone catches 29% of these errors.
- Review interactions and allergies - Cross-check with their full medication list. A patient on warfarin who just got a new prescription for ibuprofen? That’s a dangerous combo. Counseling catches this 71% of the time.
Research shows that spending just 2.3 minutes on counseling reduces errors by 12.7% for every extra 30 seconds. A 90-second session cuts errors by 47%. That’s not luck. That’s science.
Open Questions Beat Closed Ones
The way you ask matters. Closed questions like "Is this for your blood pressure?" get a yes or no. Open questions like "What do you understand this medication is for?" get real answers. Pharmacy Times found that open-ended questions identify 3.2 times more errors than yes/no questions.Imagine this:
- Closed: "Are you taking this for cholesterol?" → Patient says "Yes." But they’re actually supposed to be on a different statin. Mistake missed.
- Open: "Tell me what your doctor told you about this pill." → Patient says, "I thought it was for my cholesterol, but my last one was blue. This one’s orange." → Mistake caught.
It’s not about tricking patients. It’s about giving them space to speak. And when they do, they often catch errors themselves.
Who Benefits Most From Counseling?
Not all patients are equally vulnerable. The highest-risk groups are the ones where counseling makes the biggest difference:- Patients over 65 - Dosing errors are 3.7 times more likely to cause serious harm in older adults. A 78-year-old on 8 medications? Counseling is critical.
- Patients with low health literacy - 42% of undetected errors happen here. If someone can’t read or doesn’t understand medical terms, they won’t know if something’s wrong.
- Those starting new high-alert medications - Insulin, opioids, blood thinners, seizure drugs. These are the ones that kill when dosed wrong. The Institute for Safe Medication Practices says 1 in 5 dispensing errors involve these drugs.
- New prescriptions - Counseling catches 91% of errors on new meds. For refills? Only 33%. Why? Patients assume it’s the same. It might not be.
That’s why the Joint Commission and CMS now require pharmacies to engage patients as safety partners. It’s not optional. It’s standard.
What’s Holding Pharmacists Back?
The data is clear: counseling works. But in many pharmacies, it’s not happening the way it should.CVS Health ran a pilot where technicians asked, "Does this look like what you’ve taken before?" They caught 1,247 errors in three months. Walgreens saw a 58% drop in errors after adopting their "Medication Checkpoint" protocol.
Yet, many pharmacists spend just 1.2 minutes per patient - half the recommended time. Why? Corporate pressure. Productivity targets. "Don’t slow down the line." One Reddit thread from a pharmacy tech said: "We’re told to get through 40 prescriptions an hour. Counseling? We barely have time to say hello."
Independent pharmacies do better. They average 78% counseling compliance versus 62% in chains. Why? Less pressure. More time. More trust with patients.
But here’s the twist: pharmacies that use structured counseling see a 19% drop in malpractice insurance premiums. Why? Fewer errors mean fewer lawsuits. The cost of counseling? About $0.87 per prescription. The cost of a single error? Up to $10,000 in liability, not to mention the human cost.

How to Do It Right: The 4-Step Framework
The APhA’s Medication Error Prevention Certificate Program gives a clear, timed structure:- Identity verification - 27 seconds. "Can I confirm your name and date of birth?"
- Purpose confirmation - 43 seconds. "What did your doctor say this is for?"
- Appearance and administration check - 52 seconds. "Here’s your pill. Does it look familiar? Show me how you’ll take it."
- Interaction and allergy review - 38 seconds. "Are you taking anything else? Any allergies?"
Total time: 2 minutes 40 seconds. That’s all it takes to catch 85% of errors - if done right.
Pharmacies that implemented this saw error detection jump from 61% to 85% in six months. The key? Training. Pharmacists need to know the indications for 200+ common drugs. They need to recognize when a patient is confused. And they need to feel empowered to take the time.
The Bigger Picture: Regulation, Cost, and Future
The federal government is catching on. CMS now ties 8.5% of Medicare Part D reimbursement to documented counseling that includes error verification. The proposed 2024 Federal Pharmacy Safety Act would require counseling for all high-alert medications. Thirty-four states already require it for opioids.And it’s paying off. Pharmacies with strong counseling protocols have 3.2 fewer errors per 10,000 prescriptions. That’s an estimated $1.7 million saved per pharmacy each year. Evaluate Pharma predicts that by 2027, pharmacies with robust counseling will gain 12-15% market share - not because they’re cheaper, but because patients trust them more.
83% of patients prefer pharmacies with thorough counseling. One review on Healthgrades said: "The pharmacist caught that my new blood thinner was the wrong strength when I said it looked smaller than before." That’s not a complaint. That’s a testimonial.
Final Thought: Counseling Isn’t Extra - It’s Essential
Technology helps. But it doesn’t replace human judgment. A machine can’t hear hesitation in a patient’s voice. It can’t notice when someone’s eyes glaze over when you say "take once daily." It can’t ask, "Why do you think this is different?" Patient counseling isn’t a nice-to-have. It’s the last, best chance to stop a mistake before it hurts someone. It’s the human firewall. And if we stop using it - not because it doesn’t work, but because we’re too busy - we’re choosing speed over safety. And that’s not a trade-off we can afford.How much time should a pharmacist spend on patient counseling to catch dispensing errors?
Research shows that pharmacists should spend at least 2.3 minutes per patient to effectively catch dispensing errors. For every additional 30 seconds spent, error rates drop by 12.7%. A structured 4-step counseling process (identity, purpose, appearance, interactions) takes about 2 minutes and 40 seconds and can raise detection rates from 61% to 85%.
Why are open-ended questions better than yes/no questions during counseling?
Open-ended questions like "What is this medication for?" encourage patients to explain in their own words, revealing misunderstandings or inconsistencies. Closed questions like "Is this for your blood pressure?" often get a simple yes, even if the patient is wrong. Studies show open-ended questions identify 3.2 times more errors than closed ones.
Can pharmacy technicians help with patient counseling for error detection?
Yes. In 42 states, pharmacy technicians are permitted to perform preliminary counseling under pharmacist supervision. This frees up pharmacists to focus on complex cases and high-alert medications. When technicians handle initial checks, effective counseling time increases by 37%, improving error detection without increasing pharmacist workload.
What types of medications are most often misdispensed, and how does counseling help?
High-alert medications like insulin, opioids, blood thinners, and seizure drugs are most commonly misdispensed. The Institute for Safe Medication Practices reports that 1 in 5 dispensing errors involve these drugs. Counseling catches these errors by verifying the patient’s recognition of the medication’s appearance, purpose, and dosage - things automated systems often miss.
Do patients really notice when a medication looks different?
Yes. Studies show that asking patients if the medication looks familiar catches 29% of look-alike errors. One patient noticed their new blood thinner pill was smaller than before - it turned out to be the wrong strength. That kind of observation is impossible for machines to detect, but patients often notice changes in size, color, or shape.
Is patient counseling cost-effective for pharmacies?
Yes. Counseling costs about $0.87 per prescription, compared to $1.35 for barcode systems and $2.10 for pharmacist double-checks. Pharmacies using structured counseling report 19% lower malpractice insurance premiums and avoid an estimated $1.7 million in error-related costs per year. It’s the most cost-effective error-detection method available.

 Pharmacology
Pharmacology